Oesophageal Balloon
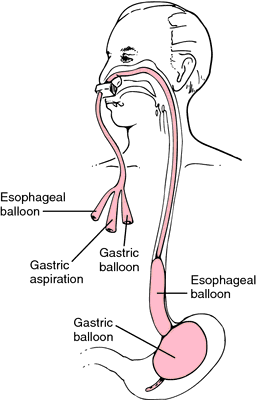
Oesophageal balloons include the Linton-Nachlas (Linton) tube, Sengstaken-Blakemore (Blakemore) tube, and Minnesota tube, which differ in the number and size of the balloon(s).
Oesophageal balloon tamponade is used for temporisation of massive variceal haemorrhage until definitive treatment (generally endoscopy, occasionally TIPS) can be performed.
Indications
- Massive variceal haemorrhage
Use has substantially ↓ with improved access to endoscopy. Provides control of up to:- 92% of oesophageal haemorrhage
- 88% of gastric haemorrhage
Contraindications
- Non-secure airway
- Controlled variceal haemorrhage
- Oesophageal rupture
Boerhaave syndrome. - Oesophageal stricture
- Unclear source of bleeding
Oesophageal tamponade should only be performed on an intubated patient.
Anatomy
- The oesophagus is usually ~25cm long
- Varices occur secondary to portal hypertension, and may form in the:
- Distal third of the oesophagus
- Gastro-oesophageal junction
- Gastric fundus
- Gastric antrum
Equipment
- PPE
High volume haematemesis. - Laryngoscope
- Oesophageal balloon
- Lubricant
- 50mL syringe
- Stopcocks
- Luer-lock caps
- Pressure manometer
As used for ETT cuff inflation. - Portable XR
- 500mL-1L saline
Or similar, for traction. - Crepe bandage
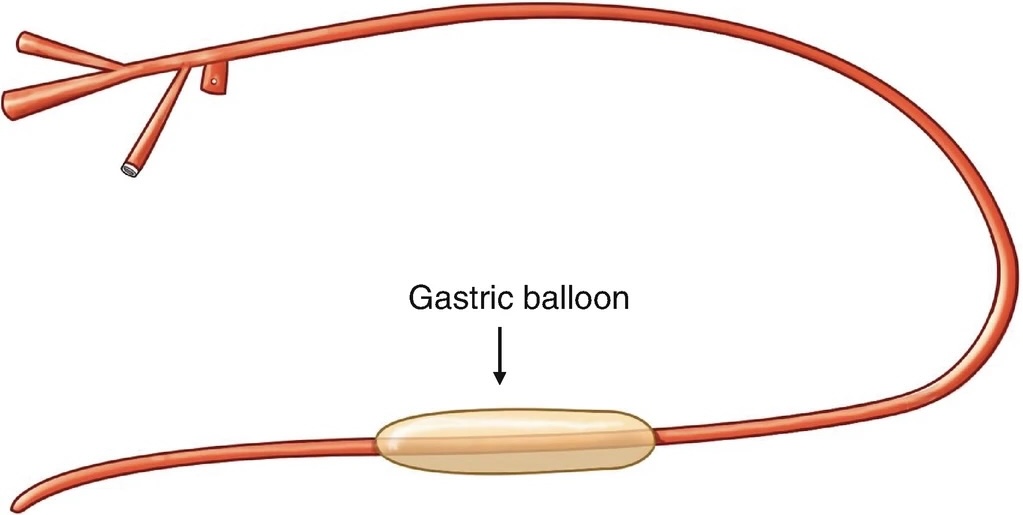
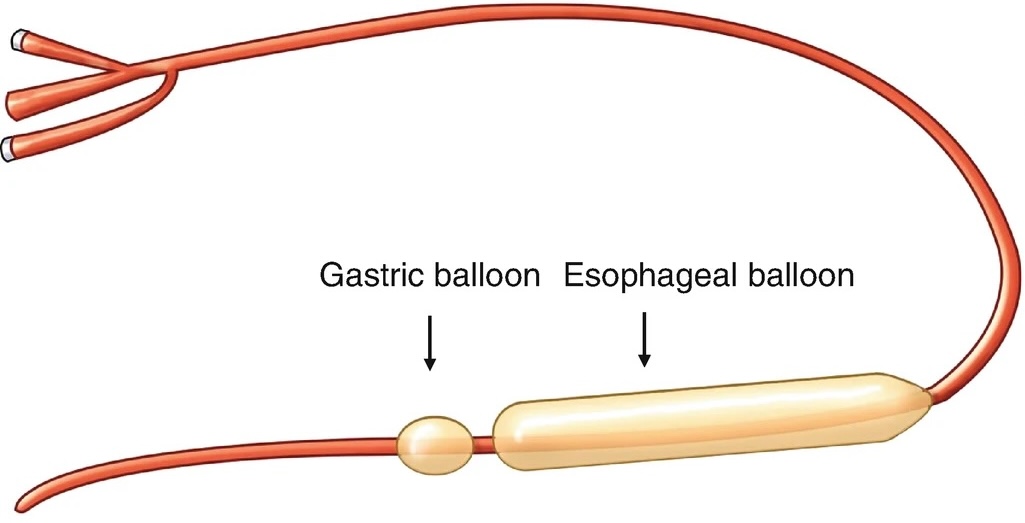
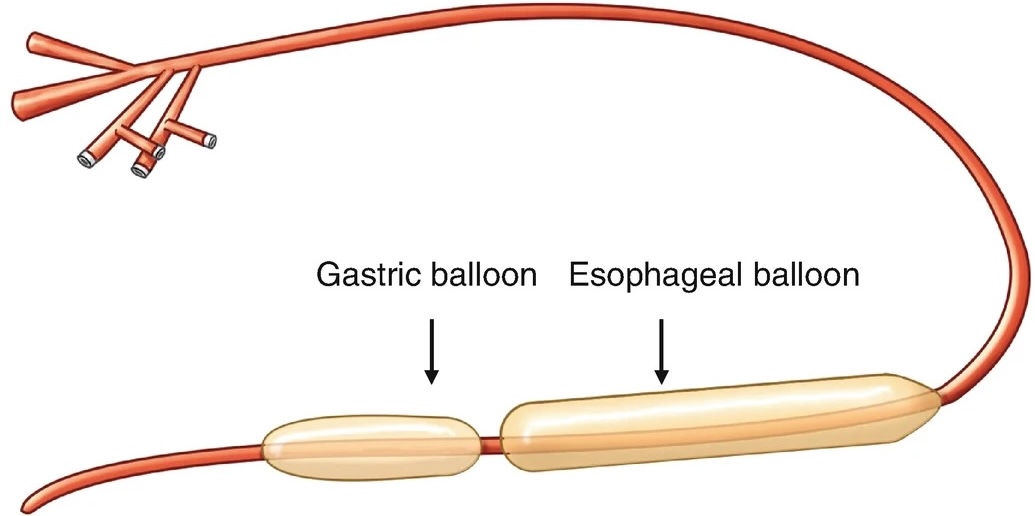
| Property | Linton-Nachlas | Sengstaken-Blakemore | Minnesota |
|---|---|---|---|
| Balloons |
|
|
|
| Ports |
|
|
|
| Other |
|
Technique
Inflation of the gastric balloon in the oesophagus is usually fatal. Ensure the device is seated correctly in the stomach before inflating the oesophageal balloon.
Preparation:
- Sit the patient at 45°
↓ Aspiration risk. - Check each balloon for leaks by underwater inflation
- Thoroughly lubricate each balloon
Tubes can be placed nasally, and historically this seems common. However, in general oral placement is preferred as the patient is:
- Intubated
Or should be, given the high risk of aspiration. - Coagulopathic
- Thrombocytopaenic
Insertion:
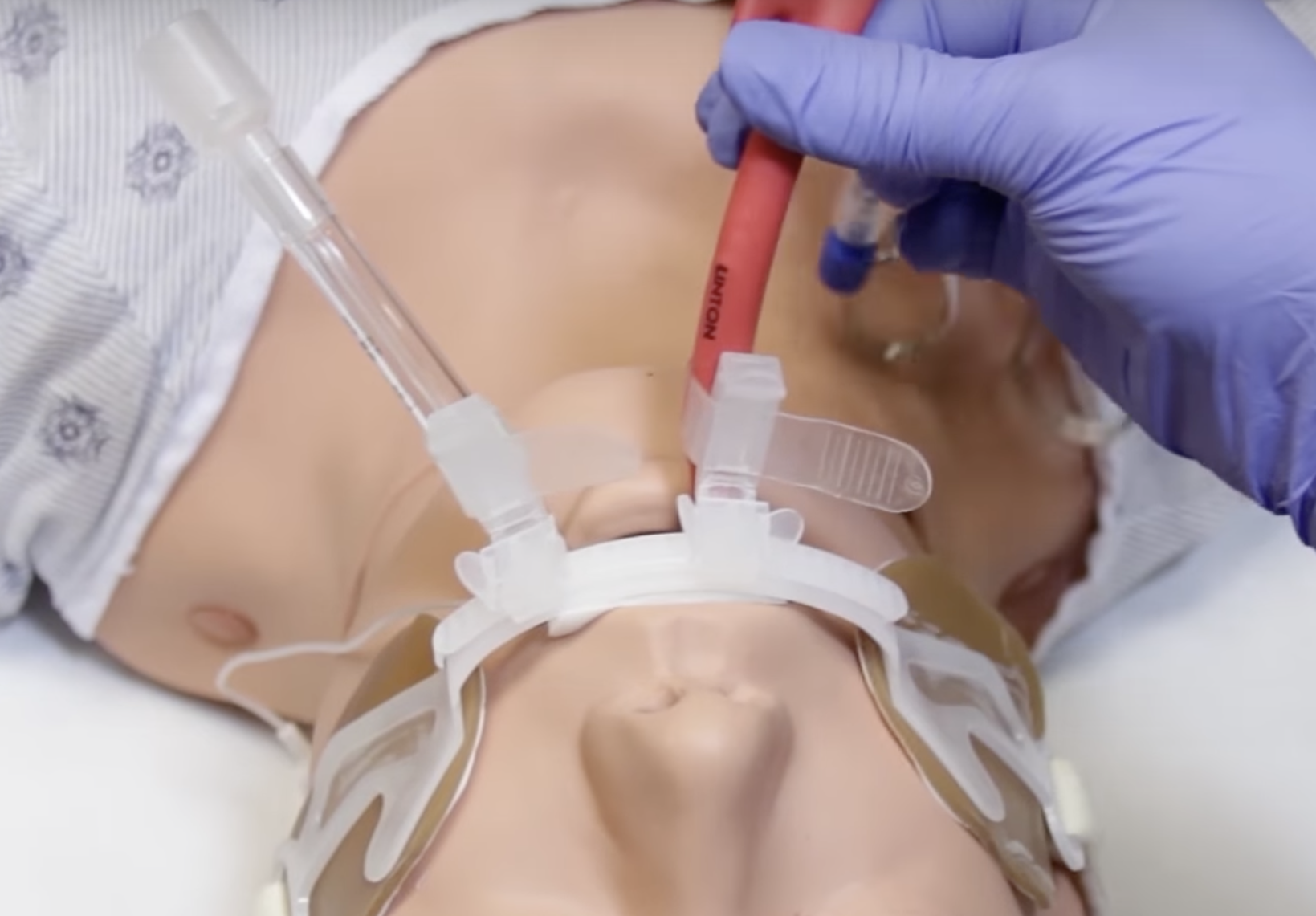
- Insert the tube via the mouth under laryngoscopic guidance to 50cm
- Inflate the gastric balloon with 50-100mL of air
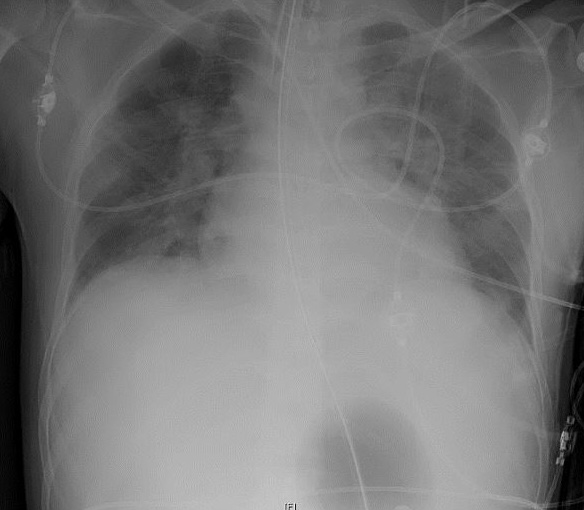
- Confirm position of the gastric balloon under the diaphragm with CXR
- Fully inflate gastric balloon
See the above table for the total volume. Use a stopcock to prevent gas leaking out whilst insufflating the tube. - Gently retract balloon back against the gastric fundus until resistance is felt
Usually at 30-35cm. - Tie crepe bandage to balloon and to bag of saline, and then perform traction using the bed pole.
- Secure the balloon in location
Consider using an additional connector on the endotracheal tube fastener. - Attach medium suction to gastric port
60-100mmHg suction. - Attach high suction to oesophageal port
120-150mmHg.

Oesophageal Tamponade:
- Gastric fundal tamponade is usually adequate; oesophageal inflation should only be used if there is continual bleeding despite an adequately inflated and tensioned gastric balloon
- Inflate oesophageal balloon to 25-30mmHg
- Deflate balloon by 10mmHg Q2H once bleeding has resolved
Removal:
Local protocols may vary, this describes one method for staged removal.
- Fully deflate the oesophageal balloon
- Monitor for 4-6 hours
- Release tension on the gastric balloon
- Monitor for further 4-6 hours
- Deflate the gastric balloon
- Monitor for further 4-6 hours
- Gastric aspirates for blood volume
- Haemodynamic stability
- Remove the tube
Complications
This is a morbid procedure; overall complication rate is ~20%.

- A
- Aspiration
- C
- Cardiac compression
- D
- Pain
- G
- Oesophageal perforation
- Pressure necrosis
- Deflate after 12 hours
- Do not use longer than 24-36 hours
References
- Lee BT, Kahn JA. Balloon Tamponade for Variceal Hemorrhage. In: Demetriades D, Inaba K, Lumb PD, editors. Atlas of Critical Care Procedures [Internet]. Cham: Springer International Publishing; 2018 [cited 2023 Oct 12]. p. 283–8.
- Birse DRB. Inferolateral ST-segment elevation associated with a gastric variceal bleed and the use of a Minnesota tube. Case Reports. 2014 Jan 20;2014(jan20 1):bcr2013202795–bcr2013202795.
- Mason, J. Placement of a Linton tube for Bleeding Varices. EM:RAP Productions. Youtube. 1 Apr 2016.