Fluid
Fluid resuscitation and administration is a cornerstone of critical care medicine. Key considerations include:
This covers consideration for fluid administration and resuscitation, considerations of management of volume state in the critically ill is covered under Volume State.
- Epidemiological
- Critically unwell patients typically:
- Receive large volumes of fluid
- Retain large volumes of fluid
- Positive fluid balance correlates with mortality
- ICU patients tend to be euvolaemic by the time of admission
- Critically unwell patients typically:
- Phase of Illness
- Resuscitation phase often requires fluid administration and tolerance of positive fluid balance
- Maintenance and recovery phase requires attention to de-resuscitation
- Minimise use of maintenance fluids
- Control of volume state
- Appropriate management of hypernatraemia
- Choice of fluid
- Crystalloid
- Colloid
Contains microscopic particles that are large enough to be retained within the vascular compartment. Include:- Albumin
- Synthetic
Gelatins and starches are not recommended due to a variety of adverse reactions including:- Hypersensitivity
- AKI
- Coagulopathy
- Crystalloid
Crystalloid
Isotonic Bicarbonate
- Consider for hypovolaemia with concurrent NAGMA or uraemic acidosis
- Preparation:
- Remove 160mL from 1L of sterile water or D5W, leaving 840mL
- Add 160mL of 8.4% NaHCO3 to the bag
- Administer within 12 hours as it is not stable in a plastic fluid bag
Colloid
The volume-expanding effect of colloid is ↓ in the critically ill, presumably due to ↑ endothelial permeability and glycocalyx disruption.
Albumin
Human albumin solution is produced from human plasma, and:
Physiological effects of albumin include:
- Major protein responsible for colloid oncotic pressure
- Anti-inflammatory
- Free radical scavenging
- Buffer
- May be presented as solution of:
- 4% Albumin
Cost-free by-product of PRBC production, exclusive to Australia. - 5% Albumin
Isotonic solution. - 20% Albumin
Hypertonic solution used for both:- Hypoalbuminaemia
- Fluid overload
- 4% Albumin
- Has risks of:
- Creutzfeldt-Jakob disease
- Has no proven benefit over crystalloid
Risk of HIV or hepatitis is not present with albumin solutions due to heat treating of product.
Key Studies
Balanced Crystalloids:
Overall, I have:
- A strong preference for 0.9% saline as the default fluid in neurosurgical patients, based on a weak foundation of secondary outcomes and sub-group analyses showing ↑ mortality with hypotonic and ↓ [Na+] solutions
- A weak preference for balanced crystalloids in the remainder of the ICU population
- A strong belief that fluid trials will never demonstrate superiority of one solution over another in the general ICU population, due to:
- Most patients will not have their outcome changed (in any direction) by the choice of IVT
Most will either be too well or too sick for it to matter. - If any do, there is probably heterogeneity in the effect of fluid in different subgroups
- Clinicians will attempt to reverse any adverse effects (AKI, acidosis) seen
- Most patients will not have their outcome changed (in any direction) by the choice of IVT
- Critical care patients routinely receive IV fluid
- If one fluid is superior, even very small benefits translate to a significant impact due to the number of patients receiving the therapy
- Saline is historically the most common, but there are concerns that the chloride load contributes to acidosis, ↓ renal cortical blood flow, ↑ need for RRT, and ↑ mortality
- SPLIT (2015)
- 2278 Kiwis admitted to ICU requiring crystalloid, without ESRD or anticipated need for RRT
- Randomised, multicentre (4), feasibility study
- Plasmalyte 148 vs. 0.9% saline
- No change in AKI (9.6% vs 9.2%) by RIFLE
- Secondary outcomes showed no difference in AKI, duration of organ support, or death
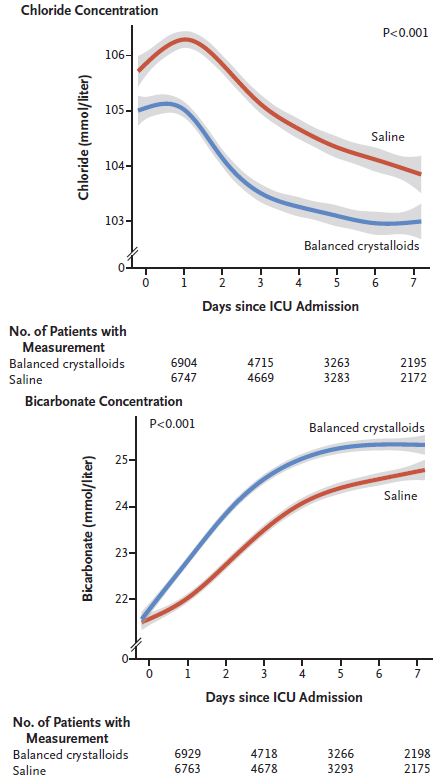
- SMART (2018)
- ~16,000 adult Americans admitted to ICU
- Unblinded, cluster-randomised, single-centre (but multiple ICU, multiple crossover trial
ICU randomised to either 0.9% saline or a balanced crystalloid, and altered fluid each month. Associated ED and OR were given the same fluid, except for cardiac surgery patients. - 14,000 patients gives 90% power to detect 1.9% ↓ in major adverse kidney events at 30 days, from 15% in saline group
Composite outcome of death, RRT, or persistent renal dysfunction (last inpatient creatinine >200% of baseline). Censored at 30 days or discharge. - Balanced vs. normal saline
- Balanced
- Plasmalyte vs. lactated Ringer’s
- Normal saline could be given if hyperkalaemic or TBI
- Balanced
- ↓ Primary outcome in balanced group (14.3% vs. 15.4%, OR 0.91 (CI 0.84-0.99))
- Secondary outcomes show no difference in any of the components of subgroup analyses
- Patients in ICU over the end of a calendar month may have received both therapies
It is worth noting that hyperkalaemia should not be an exclusion to balanced crystalloids; the acidosis generated from administration of saline results in a greater ↑ in serum [K+] than the potassium content of a balanced solution does.
- PLUS (2022)
- 5037 non-pregnant Australasians without TBI or a specific fluid requirement who required fluid resuscitation, had some sort of invasive line, and were anticipated to be >3 days in ICU
- Initially planned for 8800 patients, powered at 90% for a 2.9% ARR in 90 day mortality
- 23% control group mortality
- 2% loss to followup
- Revised to 5000 patients at start of COVID-19 pandemic as non-COVID research suspended and funding diverted
90% power for 3.8% ARR in 90 day mortality.
- Initially planned for 8800 patients, powered at 90% for a 2.9% ARR in 90 day mortality
- Investigator-initiated, double-blinded, parallel-group, multicentre (53), block-randomised RCT
- Saline vs. Plasmalyte 148
- Saline group
- 3.7L saline received over 6 days
- 3.5% received >500mL plasmalyte
- Plasmalyte group
- 3.9L plasmalyte received over 6 days
- 63% received >500mL saline
- Saline group
- No difference (21.8% vs 22%) in 90-day mortality
- 5037 non-pregnant Australasians without TBI or a specific fluid requirement who required fluid resuscitation, had some sort of invasive line, and were anticipated to be >3 days in ICU
- BASICS (2018)
- 11,000 Brazilians admitted to ICU requiring fluid resuscitation with some risk factor for AKI, without profound electrolyte derangements or imminent need for RRT or palliative care
- 89% power for hazard ratio of <0.9, assuming 35% control mortality
- 2x2 factorial study evaluating two primary outcomes:
- Fluid type
Plasmalyte vs. saline:- No difference in 90 day mortality (26.4% vs 27.2%)
- Significant ↑ mortality in TBI sub-group (31% vs 21%, CI 1.03-2.12)
- Significantly ↓ SOFA in plasmalyte group (26% vs. 32%)
- No difference in 90 day mortality (26.4% vs 27.2%)
- Speed of infusion
Slow (333mL/hr) vs. fast (999mL/hr) infusion of fluid boluses.- No difference in 90 day mortality
- Fluid type
- Both studies block randomised
- Randomised fluid type and rate used for entire ICU stay unless contraindicated
- Blood, albumin, and bicarbonate permitted
- Mortality lower than expected, ↓ power
Albumin:
- SAFE (2004)
- ~7000 Australian adult ICU patients requiring fluid administration, excluding post-cardiac surgery, liver transplant, and burns
- Multicentre, double-blinded RCT, stratified by trauma diagnosis and site
Special fluid administration sets were used to hide the albumin. - 4% albumin vs. 0.9% saline
- No change in 28-day mortality (20.9% vs. 21.1%)
- No statistically significant difference in ICU length of stay, duration of organ support. However:
- Trauma subgroup had an almost significant ↑ mortality (13.6% vs. 10%, RR 1.36 (CI 0.99-1.86))
- Sepsis subgroup had a more insignificant ↓ mortality (30.7% vs. 35.3%, RR 0.87 (CI 0.74-1.02))
- Trauma subgroup had an almost significant ↑ mortality (13.6% vs. 10%, RR 1.36 (CI 0.99-1.86))
- Less cumulative fluid balance at end of day 1 and 2 in the albumin group (by ~1:1.4), although this difference started resolving at day 3 and had gone at day 4
Note that 4% Albumin is hypotonic at 260mOsmol/L. This may contribute to the poor outcomes seen in the neurosurgical group, and is explored elegantly by Iguchi et al.
- ALBIOS (2014)
- 1818 Italians within 24 hours of severe sepsis, without head injury, heart failure, or specific indication for albumin
- Multicentre (100) open-label, randomised trial, with stratification by ICU and time of sepsis onset
- 80% power for 7.5% ARR (!) ↓ in 28-day mortality, with control mortality of 45%
- 20% albumin vs. crystalloid
- 20% albumin
- 300mL 20% albumin on randomisation
- Further 20% targeting serum albumin >30g/L
- Crystalloid as clinically indicated
- Crystalloid
- Crystalloid as clinically indicated
- 20% albumin
- No mortality difference (31.8% vs. 32%)
- 20% albumin is safe and improves haemodynamics, but does not provide a survival advantage
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.
- Finfer S, Micallef S, Hammond N, et al. Balanced Multielectrolyte Solution versus Saline in Critically Ill Adults. New England Journal of Medicine. 2022;386(9):815-826. doi:10.1056/NEJMoa2114464
- Zampieri FG, Machado FR, Biondi RS, et al. Effect of Slower vs Faster Intravenous Fluid Bolus Rates on Mortality in Critically Ill Patients: The BaSICS Randomized Clinical Trial. JAMA. 2021;326(9):830-838.
- Zampieri FG, Machado FR, Biondi RS, et al. Effect of Intravenous Fluid Treatment With a Balanced Solution vs 0.9% Saline Solution on Mortality in Critically Ill Patients: The BaSICS Randomized Clinical Trial. JAMA. 2021;326(9):818-829.
- Semler MW, Self WH, Wanderer JP, et al. Balanced Crystalloids versus Saline in Critically Ill Adults. New England Journal of Medicine. 2018;378(9):829-839. doi:10.1056/NEJMoa1711584
- Young P, Bailey M, Beasley R, et al. Effect of a Buffered Crystalloid Solution vs Saline on Acute Kidney Injury Among Patients in the Intensive Care Unit: The SPLIT Randomized Clinical Trial. JAMA. 2015;314(16):1701-1710. doi:10.1001/jama.2015.12334
- Jaber S, Paugam C, Futier E, et al. Sodium bicarbonate therapy for patients with severe metabolic acidaemia in the intensive care unit (BICAR-ICU): a multicentre, open-label, randomised controlled, phase 3 trial. The Lancet. 2018;392(10141):31-40. doi:10.1016/S0140-6736(18)31080-8
- A Comparison of Albumin and Saline for Fluid Resuscitation in the Intensive Care Unit. New England Journal of Medicine. 2004;350(22):2247-2256. doi:10.1056/NEJMoa040232