Methaemoglobinaemia
Methaemoglobin is an altered form of haemoglobin where the normal ferrous (Fe2+) iron of haeme become oxidised to the ferric (Fe3+) state, and unable to bind oxygen.
Methaemoglobinaemia is a methaemoglobin level >1.5%.
Epidemiology and Risk Factors
Pathophysiology
Methaemoglobinaemia occurs due to oxidation of the iron in haeme, and:
- Occurs normally
Usually 0.5-3% of total haemoglobin per day.
Aetiology
- Congenital
- Cytochrome B5 reductase deficiency
- Acquired
- Drugs
- Nitrites
- NO
- SNP
- Amyl nitrite
- Metoclopramide
- Prilocaine
- Benzocaine
Common adulterant in street cocaine. - Chloroquine
- Dapsone
- Nitrites
- Drugs
Assessment
Features relate to impaired oxygen transport:
- Cyanosis
This is paradoxical, as the SpO2 will generally be ~85% - too high to cause cyanosis. - ↓ DO2
- Angina
- Dyspnoea
- Confusion → obtundation
- SpO2 85-90%
| Level | Features |
|---|---|
| <2% | - |
| 3-15% |
|
| 20-30% |
|
| >40% |
|
History
Exam
Investigations
Bedside:
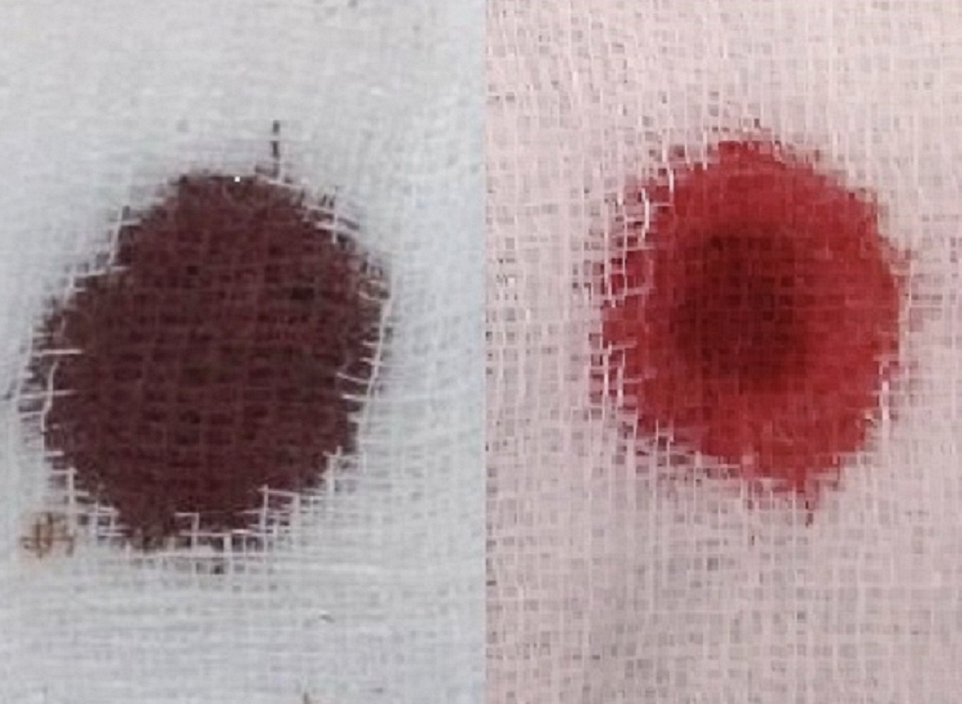
- Brown blood test
Brown discolouration of blood will remain unchanged as it clots. Normal blood will redden as it uptakes oxygen from the atmosphere. - Pulse oximetry
Typically reads 82-86%, independently of the true PaO2. - ABG
- Normal PO2
- ↑ MetHb
Laboratory:
- Blood
- MetHb levels
Imaging:
Other:
Diagnostic Approach and DDx
Management
- Supplemental oxygen
- Reduction of methaemoglobin
Resuscitation:
- B
- Supplemental oxygen
Specific therapy:
If methylene blue fails, consider:
- Ongoing exposure
- Sulfhaemoglobinaemia
- Sulfonamides
- Dapsone
- G6PD deficiency
See G6PD Deficiency. - Haemoglobinopathy
- Excessive methylene blue
- Pharmacological
- Reduction agents
- Methylene blue 1-2mg/kg over 5 minutes
- Artificial electron receptor, reduces MetHb by an NADPH dependent pathway
This requires G6PD, and will produce haemolysis in patients with G6PD deficiency. - Indicated for:
- Symptomatic methaemoglobinaemia
- Asymptomatic and:
- MetHb >10% and vulnerable to ischaemia
- MetHb >20%
- Can repeat in 30-60 minutes
- May induce methaemoglobinaemia in high doses
- Contraindicated in:
- G6PD
- Serotonin syndrome
- Artificial electron receptor, reduces MetHb by an NADPH dependent pathway
- Ascorbic acid 1.5-3g IV Q6H
- NAC
- Methylene blue 1-2mg/kg over 5 minutes
- Reduction agents
- Procedural
- Exchange transfusion
- Hyperbaric oxygen
- Physical
Supportive care:
Disposition:
Preventative:
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
Prognosis
Key Studies
References
- Paul A, Chacko ST. Congenital methaemoglobinaemia diagnosed in an adolescent boy. BMJ Case Rep. 2019 Mar;12(3):e228470.