Idiopathic Interstitial Pneumonia
Group of diffuse parenchymal lung diseases of unclear aetiology that are characterised by:
- Expansion of the pulmonary interstitial compartment
- Inflammatory infiltrate
This classification encompasses a a number of subsidiary interstitial diseases including:
Acute interstitial pneumonia is also known as Hamman-Rich syndrome.
- Acute interstitial pneumonia
Variant characterised by:- Acute onset
7-14 days. - Rapidly progressive course
Generally require intubation within a few days. - Diffuse lung injury
- Acute onset
- Organising pneumonia
Inflammatory lung disease characterised by granulation in small airways and alveoli. Subdivided into:- Cryptogenic organising pneumonia
No obvious cause. - Secondary organising pneumonia
Following previous alveolar injury, including:- Post-infectious
See below. - Drugs
- Connective tissue disorders
- Rheumatoid arthritis
- Systemic sclerosis
- Lupus
- Inflammatory bowel disease
- Vasculitis
- Granulomatosis with polyangitis
- Eosinophilic granulomatosis with polyangitis
- Transplantation
- Malignancy
- Haematological
- Radiotherapy
- Thoracic malignancy
Generally 3-6 months.
- Thoracic malignancy
- Chemotherapy
- Allogenic BMT
- Industrial chemical exposure
- Post-infectious
- Cryptogenic organising pneumonia
- Lymphoid interstitial pneumonia
Cryptogenic organising pneumonia was formerly known as bronchiolitis obliterans organising pneumonia (BOOP).
Epidemiology and Risk Factors
AIP:
- Associated with:
- Rheumatoid arthritis
- SLE
- Dermatomyositis
- Sjögren’s syndrome
COP:
- ~1-5/100,000
Pathophysiology
Poorly understood, features include:
- Inflammation
- Intra-alveolar fibroproliferation
- May be reversible
- Fibrinous remodelling
Aetiology
| Infection | Drug |
|---|---|
Bacteria:
|
Common:
|
Viruses:
|
Immune and cancer:
|
Parasites:
|
Recreational:
|
Fungi:
|
Chemical:
|
Atypical infections are more likely to be the primary precipitant.
Clinical Features
Typically subacute presentation with:
- Dry cough
- Progressive dyspnoea
- Constitutional symptoms
- Fever
- Malaise
- Weight loss
| Cause | Onset | Cough |
|---|---|---|
| AIP |
|
|
| COP |
|
|
Assessment
History
Exam
- Bilateral diffuse crepitations
Investigations
Bedside:
- Bronchoscopy
- BAL
To evaluate for eosinophilic pneumonia and alveolar haemorrhage.
- BAL
Laboratory:
- Blood
- FBE
Mild leukocytosis is common. - BNP
Exclude CCF. - Cultures
- Rheumatological screen
- Connective tissue disease screen
- FBE
- Sputum
- Culture
- Fungal
- Atypical organisms
- Viral PCR
- Influenza
- Culture
- Urine
- Legionella PCR
A rheumatological screen consists of:
- Initial investigations:
- FBE
- UEC
- ESR
- CRP
- LFT
- ANA
- Rheumatoid factor
- Anti-CCP antibodies
- Vitamin D
- Urinealysis
- Second-line investigations
For patients with strong clinical suspicion:- Anti-synthetase antibodies
- Creatine kinase
- Aldolase
- Sjögren’s antibodies
- SS-A
- SS-B
- Scleroderma antibodies
- Anti-topoisomerase (Scl-70)
- Anti-PM-1 antibody
- Anti-centromere
- Anti-dsDNA antibodies
- Myositis-associated antibodies
- Jo-1
- PL-7
- PL-12
- ANCA
- Anti-melanoma differentiation-associated gene 5
- Overlap antibodies
PM-1.
Imaging:
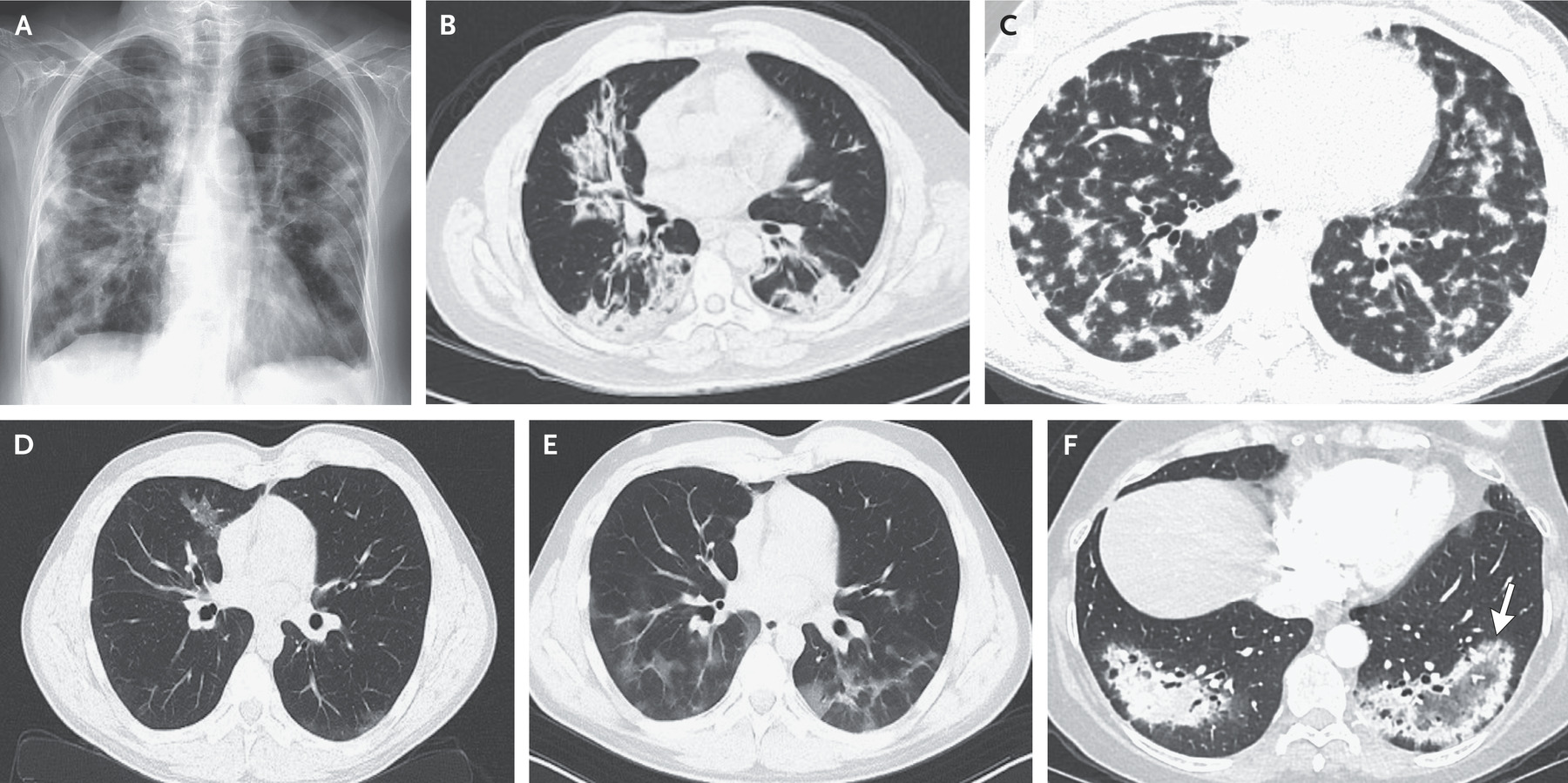
- CXR
- Consolidative opacities with normal lung volumes
Figure A.
- Consolidative opacities with normal lung volumes
- High-resolution CT
- Multifocal consolidation
- Peripheral nodulation
Figure C. - Migratory opacities are classical for organising pneumonia
Figure D and E are the same patient at different time points. - Atoll sign
Rim of consolidation with central ground-glass opacities, which is rare but highly specific.
Other:
- Bronchoscopy
- BAL
Evaluate for:- Diffuse alveolar haemorrhage
- Eosinophilia
- Malignant infiltrates
- BAL
Diagnostic Approach and DDx
Key differentials include:
- CAP
Absence of antibiotic response suggests organising pneumonia. - Hypersensitivity pneumonitis
- Eosinophilic pneumonia
- Diffuse Alveolar haemorrhage
- Vasculitis
- Pulmonary lymphoma
- Invasive mucinous adenocarcinoma
- Pulmonary sarcoidosis
Management
- Broad-spectrum antimicrobials
- Immunosuppression with corticosteroids
Resuscitation:
Specific therapy:
- Pharmacological
- Antibiotics
Commenced empirically until infectious causes are excluded. - Corticosteroids
1mg/kg prednisolone daily up to 60mg per day, for 2-4 weeks followed by a 3-5 month taper.
- Antibiotics
- Procedural
- Lung transplantation
- Physical
Supportive care:
Disposition:
Preventative:
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
- Death
- AIP
~50% by 6 months.
- AIP
- B
- Chronic interstitial lung disease
- Relapse
- Particularly with organising pneumonia
Prognosis
Key Studies
References
- King TE, Lee JS. Cryptogenic Organizing Pneumonia. New England Journal of Medicine. 2022;386(11):1058-1069. doi:10.1056/NEJMra2116777
- Mrad A, Huda N. Acute Interstitial Pneumonia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 Sep 30].