Surroundings
The ICU environment provides several clues to diagnosis and severity of illness. Key regions include:
- Bedspace
- Monitor
- Ventilator
- Infusions
- Lines and drains
- IDC
- NG
- Faecal management system
- Surgical
- Ancillary equipment
Bedspace
- Isolation room
- Positive pressure
- Negative pressure
- Infection control and PPE
- Waste disposal
- Cytotoxic
- Room temperature
Burns. - Medications
- Antibiotics
Implications for causative organism or resistance patterns. - Pathognomonic medications
- Antibiotics
- Long-stay
- Photographs/art
- Physical therapy equipment
- Activity plans
- Equipment
- Wheelchair
- Walking aids
- Handweights
- Splints
- Cooling blanket
Monitor
- ECG
Rate and rhythm.- HR <30-35 may lead to critical coronary hypoperfusion, independent of blood pressure
- Pressure monitoring
- Alignment to haemodynamic supports
- MAP <35mmHg (+/- 10mmHg) is usually the critical threshold for coronary perfusion, below which heart rate and cardiac output fall rapidly
- EtCO2
- Level
- Trace
- PaCO2 gradient and dead space
- Temperature
- ICP
If transduced from EVD, ensure monitor is leveled appropriately.
Integration
Patterns:
Information from the monitor, ventilator, and medications should be combined to form a clinical impression.
e.g. “The SpO2 is 93% with an FiO2 of 50% - there is evidence of a raised A-a gradient”.
Or, “The patient is in AF, I note the heparin infusion and wonder if this is the sole indication for anticoagulation.”
- Cushing Triad
↑ ICP leads to a sympathetic surge aimed to maintain cerebral perfusion, which manifests as:- Arterial hypertension
- Bradycardia
- Irregular respiration
| Type of Shock | MAP | CVP | CI/ | MPAP | PCWP |
|---|---|---|---|---|---|
| Hypovolaemic | ↓/- | ↓ | ↓ | ↓ | ↓ |
| Obstructive | ↓ | ↑ | ↓ | ↑ | ↑/- |
| Distributive | ↓ | ↓ | ↑ | ↓ | ↓ |
| Cardiogenic: LV failure | ↓/- | ↑/- | ↓ | ↓/- | ↑ |
| Cardiogenic: RV failure | ↓/- | ↑ | ↓ | ↑/-/↓ | - |
Ventilator
- Mode
- Oxygenation
- FiO2
- PEEP
- Quick assessment of A-a gradient based on SpO2 and FiO2
- Ventilation
- Minute ventilation
- Dynamic compliance
- Peak pressure
- Plateau pressure
- Consider assessing plateau pressure to determine static compliance if dynamic compliance is ↓
- Disease-specific ventilation strategies
- “Extubatable settings?”
- Airway suction
- Yellow, brown, green, or creamy
Infection. - Foamy or foamy-bloody
Pulmonary oedema. - Bloody
Tracheal suction trauma or haemorrhage. - Brown
Enteral nutrition or infection.
- Yellow, brown, green, or creamy
The colour of purulent secretions does not accurately predict the causative organism. However, in general, secretions that are:
- Yellow, brown, or putrid
Suggest bacterial infection of the lower airways or parenchyma. - Foul-smelling and yellow or dark-green
Suggest lung abscesses or bronchiectasis.
Infusions
- IV fluid
- Vasoactives
- Heparin
- Pathognomonic drugs
- Octreotide/terlipressin
- Hypertonic saline
- Hypertonic dextrose
- Nimodipine
- Mannitol
- IVIG
- TPN
- Blood
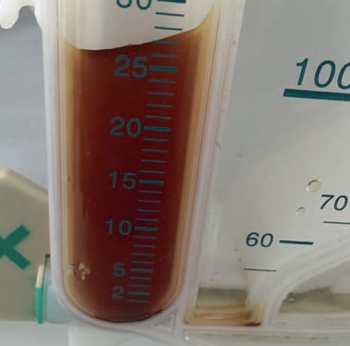
Drains
Urine
Many abnormalities of urine colour are also visible in RRT effluent.
- Quantity
- Colour
- Clear
- Polyuria
- Diabetes insipidus
- Hyperglycaemia
- Diuretic therapy
- Polyuria
- Concentrated
May indicate:- Hypoperfusion or hypovolaemia
Classically low-volume.
- Hypoperfusion or hypovolaemia
- Turbid/purulent
Pyuria suggesting infection. - Sediment
- UTI
- AKI
- Presence of IDC
- Foamy
- Proteinuria
Albuminuria secondary to nephrotic syndrome. - Urobilinogen
Dark and foamy urine secondary to hyperbilirubinaemia.
- Proteinuria
- Dark red
Frank blood suggesting macrohaematuria due to to prostate, bladder, or urethral trauma. - Rose-coloured
Suggests microhaematuria due to intravascular haemolysis. - Tea-coloured
- Glomerulonephritis
- Haemolytic crisis
- Myoglobinuria
- Blue-green
- Methylene blue
- Propofol
- Bright red without blood
Drug effects, including:- Rifampicin
- Ibuprofen
- Hydroxocobalamin
- Porphyria
- Clear
Diuretic therapy.
- Clear
Small volumes of light urine are concerning for obstruction.





Nasogastric
- Brown aspirates
Commonly occur with small bowel ileus or obstruction. - Feculent aspirates
Indicate lower intestinal obstruction or severe ileus. - Bilious aspirates
Exclude upper GI haemorrhage. - Pure nasogastric feed aspirates
Indicate gastroparesis.

External Ventricular Drain
- Set height
- Open or closed
- Colour of CSF
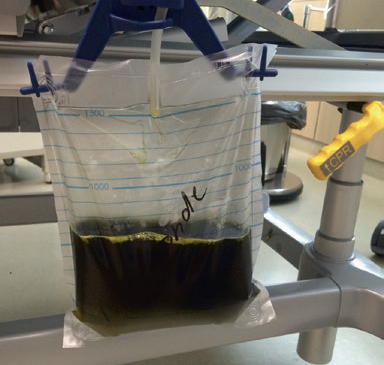
Stool
- Faecal management system
- Stool colour
- Acholic stool indicates biliary obstruction due to lack of stercobilin
- Haematochezia
- Melaena
Black, tarry, malodorous stool.- Indicates recent (4-20 hours) upper GI, small bowel, or caecal haemorrhage
- Typically becomes bloodier the more distal the bleeding source
- Stool colour

Surgical Drains
Chest:
- Location
- Pleural
- Mediastinal
- Size
- Output
- Blood
- Serous
- Behaviour
- Swinging
- Bubbling
Abdominal:

- Location
- Size
- Output
- Blood
- Serous
- Turbidity
- Bile
- Faeculent
Ancillary Equipment
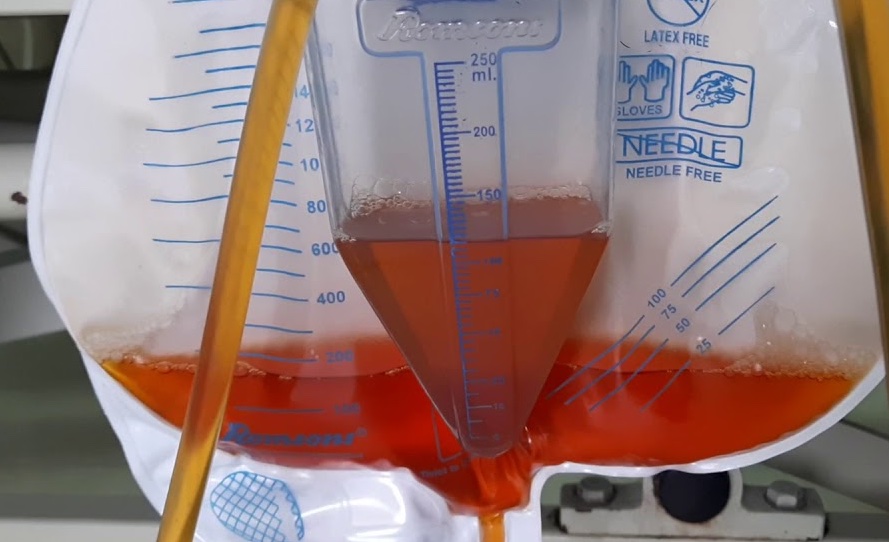
- CRRT
- Mode
- Dialysate/buffer
- Dose
- Anticoagulation
- Active cooling
- IABP
References
- Foot C, Steel L, Vidhani K, Lister B, MacPartlin M, Blackwell N. Examination Intensive Care Medicine. Elsevier Australia; 2011. (Examination series).
- Dünser MW, Dankl D, Petros S, Mer M. Clinical Examination Skills in the Adult Critically Ill Patient. Springer International Publishing; 2018.