Airway Planning
- Oxygenation > Intubation
- Optimise before you compromise
- Consider awake intubation in the presence of predictors of difficult airway
The goal of airway management is to maintain oxygenation and ventilation, without physiological compromise or complications, ideally with a patent and protected airway.
- This does not (necessarily) imply intubation
Oxygen can be delivered by:- Ventilation
- Insufflation
- Apnoeic absorption
- The chosen airway management technique will depend on the patients anatomy and physiological state, the situation, and the indication
- Secondary goals include:
- Airway protection
From aspiration. - Airway security
From dislodgement or obstruction. - Ventilation
For acidosis. - Control of airway pressures
- Control of respiratory timing
- Airway protection
The hierarchy of intubation needs: 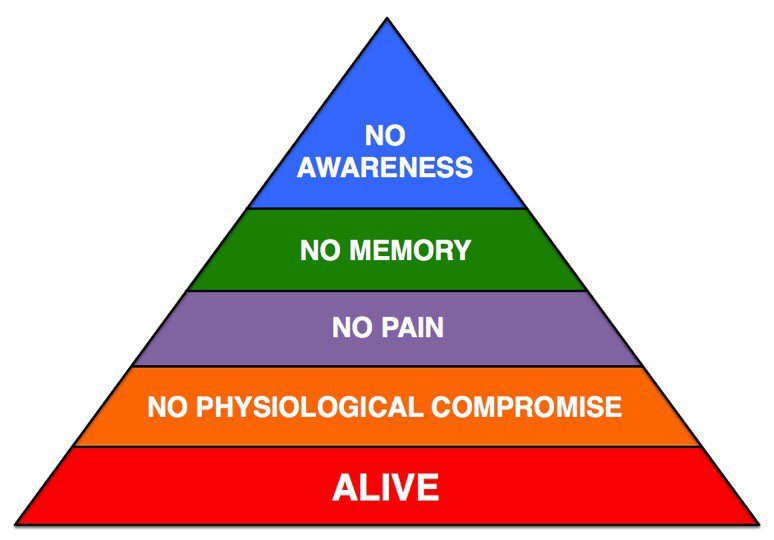
Epidemiology of Airway Complications
- The most common cause of airway related death is hypoxia
- Aspiration is the most common cause of airway related anaesthetic death
- Complications from airway management are more common in ED and ICU
- Failed tracheal intubation occurs in:
- ~1/1000-2000 elective cases
- ~1/250 obstetric RSI
- ~1/100 ED intubations
- Failed or difficult tracheal intubation was the primary event in >1/3rd of events
- CICO occurs in ~1/50,000 elective anaesthetics
- CICO is low compared to incidence of difficult intubation
- CICO contributes 25% of anaesthesia-related mortality
- Requirement for emergency FONA ↑ morbidity 15x
- ~25% permanent harm or death
- In 2/3rds of CICO situations, a surgical airway was performed too late to prevent harm
Factors Contributing to Adverse Airway Events
- Human factors
Human failures occur in ~80% of airway events.- Delayed decision to declare failed airway
- Delay in decision to perform cricothyrotomy
- Equipment knowledge
- Training
Especially in surgical airway and rescue techniques. - Poor communication
- Poor teamwork
- Tunnel vision/task focus
- Training
- Systems
- Patient Factors
- Obesity
Important technical factors include:
- Make the first attempt the best attempt
- Subsequent attempts are less successful
- Efficacy of SAD rescue is reduced with more attempts
- Equipment and technique
- Selection of laryngoscopes, and experience in their use
- Bougie
Pre-shaped. - ELM
- Remove cricoid pressure if view is poor
- Call for help early
- Maximum of 3 attempts by a single provider
A Framework for Airway Management
There are many frameworks for airway management. This one aims to:
- Focus on a general plan but not on any specific technique
- Provide an approach that is appropriate for elective anaesthesia as well as emergency airway management
- Plan for and avoid the difficult airway
- In the patient who does not require immediate intubation
- Plan
- Evaluate what techniques are available
Based on the equipment, the patient, and technical skills. Think ACORNS:- Awake
- Waking the patient
- Awake laryngoscopy
- Awake FOI
Is there laryngeal or tracheal pathology?
- Cricoid/FONA
- Scalpel cricothyrotomy
- Needle cricothyrotomy
- Oral
- Mask ventilation
- Intubation
With and without VL.
- Nasal
Is the oral route impossible?- Intubation
Including blind.
- Intubation
- Supraglotic
- Use of LMA
- Use of iLMA
- Awake
- For this patient, consider which techniques are:
- Preferred
Depending on the indication for airway management. In most critical care situations (compared to elective anaesthesia), this will be a definitive oral airway. - Feasible
Could be used to maintain oxygenation +/- ventilation, but may not necessarily be definitive. - Unfeasible
Certain techniques may not be appropriate in certain patients.
- Preferred
- Of this short-list of options, decide on a hierarchy of techniques
Plan for failure and have a series of identified rescue techniques, including a plan for:- Rescue ventilation
Alternate device, e.g. LMA, iLMA. - Rescue intubation
Alternate device.
- Rescue ventilation
- Consider which drugs will be required for these techniques
- Evaluate what techniques are available
- Patient
Adequate patient preparation prior to induction reduces incidence of difficult tracheal intubation. Think PROC:
- Positioning
- Ensure EAM is level with sternal notch to maximise ease of intubation
- Ramping ↑ FRC in the obese patient
- Recruitment
Use of CPAP during preoxygenation prolongs safe apnoea time in obese patients. - Oxygenate
Involves adequate denitrogenation, and consideration of apnoeic oxygenation.- Preoxygenation/denitrogenation
EtO2 > 80% indicates a good proportion of FRC is oxygen, significantly prolonging safe apnoea times from 1-2 minutes up to 8 minutes.- Note that reduced FRC (e.g. atelectasis) will lead to shunt and rapid drop in SpO2 despite a high ETO2 fraction
Significant shunt will result in an SpO2 of < 100% despite adequate ETO2. - This can only be achieved when breathing oxygen through a closed-circuit system
- Note that reduced FRC (e.g. atelectasis) will lead to shunt and rapid drop in SpO2 despite a high ETO2 fraction
- Apnoeic oxygenation
Delivery of oxygen via nasal cannula during the apnoeic period. This technique:- Requires a patent airway
May not help during the apnoeic period when airway tone is reduced. - May be performed with:
- Standard nasal cannula from wall oxygen at 15L.min-1
- Humidified
- May be useful when:
- FRC/ is compromised
- Laryngoscopy is difficult
- Requires a patent airway
- Preoxygenation/denitrogenation
- Perform
- Complete pre-airway management checklist
During pre-oxygenation periods. - Begin!
- Complete pre-airway management checklist
Airway Management Mental Checklist
A good mental checklist should be:
- Easy to remember
Allows it to be used as a ‘challenge-confirm’ checklist - i.e. the steps can be performed by multiple providers simultaneously and then the checklist is used to verify tasks have been completed - Appropriate to be used by a single provider as a ‘call-do-response’ checklist when working with an unfamiliar team
The SPEEDBOMB checklist:
There are many different checklists - I like this one. I routinely perform it during the pause that is provided during pre-oxygenation.
- Suction
- Available
- Consider gastric drainage if NGT is in situ
- Position
In optimal position for this particular technique.- Ear-to-sternal notch
- End-tidal CO2
Available and working. - Equipment
The kit needed for the chosen techniques.- BVM
With mask and PEEP valve. - Airway adjuncts
NPA and OPA available. - Laryngoscope
- Two working laryngoscopes
- Lubricated
Critically ill patients often have high sympathetic tone and a dry oropharynx, making advancement of an unlubricated blade down the tongue difficult. - Appropriate sized blades
- LMA
Lubed and inflated as desired. - ETT
- Of appropriate size
- Lubricated
- At least two, including a smaller one
- If concerned about upper airway pathology/burns, have a size 6 available
- Adjuncts to ETT
- Bougie
Must always be available. - Stylet
- Syringe
For cuff inflation.
- Bougie
- BVM
- Drugs
Including desired dose.- Induction agents
- Muscle relaxant
If concerned, always use adequate doses of a rapid-onset NMBD. - Opioid
- Vasopressors
- Induction agents
- Backup plan
Double check the availability of backup equipment, including FONA equipment. - Oxygen
- Supply present and connected
Ensure that the oxygen tubing attached to the flowmeter is also attached to the patient. - Adequate pre-oxygenation/denitrogenation period
- Use of PEEP for lung recruitment prior to induction
- Supply present and connected
- Monitoring
- ECG
- SpO2
- BP
- Briefing
- Allocate roles
- Detail airway plan A, B, etc
- Declare at what points the airway management strategy will change
e.g. “If the SpO2 falls to less than 93%, I will cease intubation attempts and return to BVM. If unable to mask ventilate, I will place an LMA.”
References
- Nickson, C. The challenge of the critically ill airway. 2018. CIA Course Notes.
- Mommers L, Keogh S. SPEEDBOMB: a simple and rapid checklist for Prehospital Rapid Sequence Induction. Emerg Med Australas. 2015 Apr;27(2):165-8.
- Chrimes, N. Fritz, P. The Votex Approach: Management of the Unanticipated Difficult Airway. Smashwords. 2013.
- Levitan, R. The Airway Cam Guide to Intubation and Practical Emergency Airway Management. 1st Ed. 2004.