Burns
Epidemiology and Risk Factors
Burns are:
- Common
~1% of persons.- ~10% require hospitalisation
Pathophysiology
Thermal injury results in:
- Local response
- Tissue damage
Jacksons Model:- Zone of coagulation
- Zone of stasis
Compromised but viable cells.- Amenable to treatment
- Have impaired blood flow
- Zone of stasis loss
- Inflammation
- Fluid extravasation
- Greatest in first eight hours
- Continues up to 24 hours
- Fluid extravasation
- Tissue damage
- Systemic effects
Significant when >20% BSA.- ↓ CO in first 24-48 hours
- Hypovolaemia
- ↑ Blood viscosity
- Inflammatory soup acts as negative inotrope
- ↑ CO after 72 hours
Hypermetabolic response.
- ↓ CO in first 24-48 hours
Eschar:
- Burnt dermis forming a non-elastic eschar atop of skin
- Circumferential eschar formation leads to compartment syndrome compressing oedematous tissue
Electrical burns:
- High resistance tissues produce excessive heat
- Bone generates substantial heat
Leads to muscular burns, leading to:- Rhabdomyolysis
- Fasciotomy (in addition to escharotomy)
- Rhabdomyolysis
- May have significant underlying tissue damage that is disproportionate to overlying features
- Bone generates substantial heat

Aetiology
Assessment
Burns are dynamic and will evolve and either improve or deteriorate depend on therapy
Assess:
- Depth
- Superficial
Epidermal burn.- Red and painful
- Healing within 1 week
- Not included in BSA calculation
- Superficial dermal
Dermal burn.- Blistering
- Capillary return present
- Healing is slower
- Deep dermal
- Dark red
Cooked haemoglobin locked in tissue. - May not blister
- No capillary refill
- Dark red
- Full thickness
- White/waxy/charred
- Insensate
No pain. - No blisters
- No capillary refill
No viable blood vessels. - Act as a focus for infection.
- Superficial
- Size
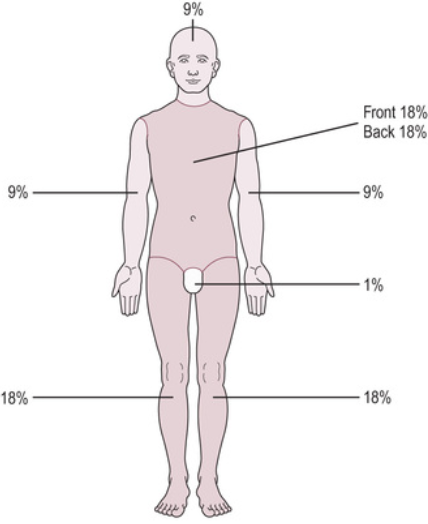
Remember to exclude superficial burns.- Rule of 9’s
- Patient palm is 1%
- Lund and Browder chart
- Rule of 9’s
History
Examination
Investigations
Diagnostic Approach and DDx
Management
- First aid and primary survey
- Transfer to burns centre
- Fluid resuscitation to moderate hypovolaemia
- Appropriate debridement and burn care
Burn patients are trauma patients and should be evaluated as such. Details of the primary survey are covered at Primary Survey.
Resuscitation:
- First aid
- Remove from heat source
- Cool the burn
Under tepid water for 20 minutes.
- A
- C
- Fluid resuscitation
Required for burns >10% in children and elderly, and >15% in adults.- Modified Parkland formula
Most commonly used protocol for burns resuscitation.- For burns >20% BSA (or 10% in children)
- 3mL/kg/% BSA burn to calculate first 24/24 fluid requirement
- Use lactated ringers or CSL
- Give half over the first 8 hours
- Titrate to urine output
- Aim 0.5-1mL/kg/hr in adults
- Aim 1-2mL/kg/hr in children
- Avoid over-resuscitation and fluid creep
Excessive volume leads to multiorgan complications- Airway occlusion
- Pulmonary oedema
- Abdominal compartment syndrome
- Consider albumin
- Fluid therapy is ↓ as enteral intake is ↑
- Modified Parkland formula
- Fluid resuscitation
Specific therapy:
- Pharmacological
- Analgesia
Multimodal:- Opioid
- Ketamine
- Analgesia
- Procedural
- Escharotomy
- Important in:
- Limbs
Compartment syndrome. - Chest
Respiratory failure. - Abdomen
Abdominal compartment syndrome.
- Limbs
- Cut down to viable tissue
Can be performed under LA as eschar is insensate. - Precise location for cut is not essential
- Tissue will ‘spring’ out as pressure released
- Important in:
- Surgical care
- Wound excision and debridement
↓ Bacterial colonisation. - Dressings
- Grafting
- May be limited by availability of unburned skin Skin can be re-harvested every ~2 weeks.
- ‘Meshing’ skin graft allows graft to be applied to skin in a 4:1 ratio
Taking skin in a ‘chicken-wire’ fashion. - Cadaveric skin can be used for temporary coverage, although autologous grafting is best
- Artificial substances:
- Biobrane
Silicone and porcine collagen.- Temporary dressing for intermediate and deep dermal burns
- Early application beneficial
Reduces tissue damage and systemic inflammatory response.
- Biodegradable Tissue Matrix
- Biobrane
- Wound excision and debridement
- Escharotomy
- Physical
Supportive care:
Burn recovery is a hypermetabolic state; energy expenditure may be doubled and significant amounts of trace elements are lost in wound exudate.
- G
- Nutrition
- Feed within 12 hours
May need 25-30kcal/kg/day due to ↑ metabolism. - Trace element supplementation
- Feed within 12 hours
- Nutrition
- H
- Thromboprophylaxis
Critical due to the high risk of VTE. Described regimens include:- Heparin 5000 units Q8H
- Enoxaparin 0.5mg/kg Q12H
- Enoxaparin Q12H, adjusted to target anti-Xa 0.2-0.4 IU/mL
- Thromboprophylaxis
- I
- Infection monitoring
Disposition:
- Transfer to burns centre if:
- ⩾10% BSA full thickness, ⩾5% in children
- Burns to key areas
- Face
- Hands
- Feet
- Perineum
- Electrical and chemical
- Inhalational injury
- Circumferential
Preventative:
Marginal and Ineffective Therapies
Anaesthetic Considerations
- A
- Airway security
May be impossible to get access again. - Facial burns
- Painful mask application
- NGT/tubes
- Airway security
- B
- Inhalational injury
- C
- Arterial line
No NIBP on burnt skin. - Fluid management
- IV access
- Ideally through unburnt skin
- Arterial line
- D
- Analgesia
Substantial pain.- Multimodal
- Early anti-neuropathics
- Single-shot regional ideal
- Analgesia
- E
- Suxamethonium contraindicated
From 48 hours to 2 years. - Temperature management
- Warm theatre
28°C. - Warming lines
- Warming CVCs
Slow rate of cooling but often unsuccessful warming. - Abandon procedure if unmanageable hypothermia (⩽35°C)
- Warm theatre
- Positioning difficult
- Suxamethonium contraindicated
- G
- Hypermetabolic
Rapid consumption of neuromuscular blockers.
- Hypermetabolic
- H
- Bleeding can be substantial
- Prepare for massive transfusion
Hard to overtransfuse.- Hb >100g/L prior to procedure ideal
- ABG every half hour to measure Hb
- Tumescent preparation
1:500,000 adrenaline infiltrated widely subcutaneously under sites prior to debridement results in substantial reduction in blood loss without adverse effect on graft success. - Bleeding will continue post-operatively
- Prepare for massive transfusion
- Coagulopathy
- Bleeding can be substantial
- I
- Sepsis
Complications
- D
- Cosmetic
- Chronic pain
- E
- Contractures
- Rhabdomyolysis
- F
- AKI
- Pre-renal
- Haemoglobinuria
- Myoglobinuria
- Hypernatraemia
- AKI
- I
- Sepsis
Often occurs due to the combination of:- Deep injuries
- Disrupted wound healing
- Immune dysfunction
- Sepsis
Prognosis
Key Studies
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.