End of Life
Patients are ‘approaching the end of life’ when they are likely to die within the next 12 months. This may be due to:
About:
- 1% of the total population die each year
- 30% of hospital patients are in their last year of life
- 80% of care home residents are in their last year of life
- 80% of people are admitted to hospital during the last year of life
- 24% have ⩾3 admissions
- Advanced, progressive, or incurable disease
- General frailty
- Condition that predisposes to death due to a sudden or acute crisis
Predicting Death
Ask yourself: ‘Would I be surprised if this patient were to die in the next few months, weeks, days’?
Most clinicians are overly-optimistic about prognostication.
Accurate prognostication of life-expectancy is difficult and therefore fraught. A better approach is to:
- Recognise the uncertainty
- Communicate clinical uncertainty to the patient and family
This can be done in a helpful way!- “While we don’t know exactly how long they may have to live, we do know that they won’t get better. Our aim is now to ensure they are comfortable, and that you are supported.”” A useful tool is to give an approximate range using common units, e.g.:
- Long weeks to short months
- Long days to weeks
- “While we don’t know exactly how long they may have to live, we do know that they won’t get better. Our aim is now to ensure they are comfortable, and that you are supported.”” A useful tool is to give an approximate range using common units, e.g.:
- Identify patients approaching the end-of-life phase
This allows for:- Better anticipation of likely care needs
- Tailoring of care to patient’s wishes
- Fewer crisis admissions
- Family and patients to plan for death
End of Life Phase
The end of life is the period when a patient is living with and impaired by a fatal condition, even if the trajectory is uncertain or unknown. It is easier to identify patients who are approaching the end-of-their life.
| Grade | Description | |
| 0 |
|
|
| 1 |
|
|
| 2 |
|
|
| 3 |
|
|
| 4 |
|
|
| 5 |
|
|
General
- Unplanned admissions
- ↓ Performance status
- ECOG >3
- Slow walking speed
>5 seconds to walk 4m. - Timed Up-and-Go
>12 seconds to stand up from the chair, walk 3 metres, turn around, and return to sitting.
- ↑ Carer support needs
- Weight loss
- Loss of muscle mass
- Cachexia
- Sentinel event
- Fall
- Bereavement
- Transfer to care facility
- Albumin <25g/L
- Advanced disease
- Unstable
- Deteriorating
- Co-morbid
- Persistent or worsening symptoms despite optimal treatment
Disease-Specific
| Disease/System | Features (⩾2 indicates ↑ risk) |
|---|---|
| Malignancy |
|
| Dementia |
|
| Cardiovascular |
|
| Respiratory |
|
| Neurological |
|
| Renal |
|
| Hepatic |
|
References
- Australian Commission for Safety and Quality in Healthcare. Comprehensive Care Standard End-of-life care: clinical basics. 2024.
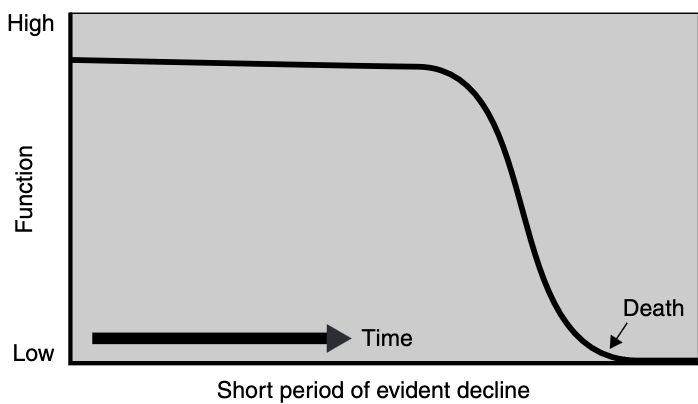
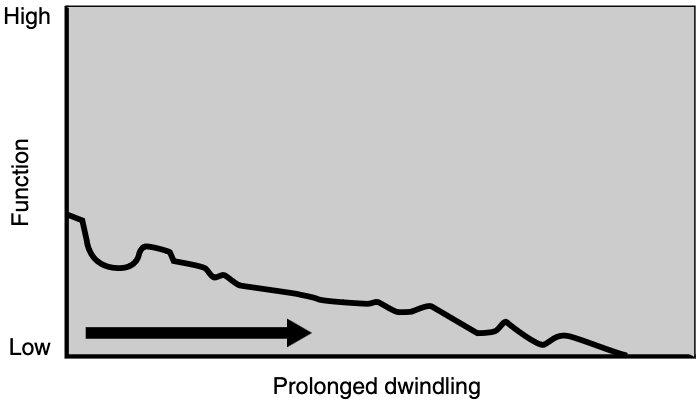
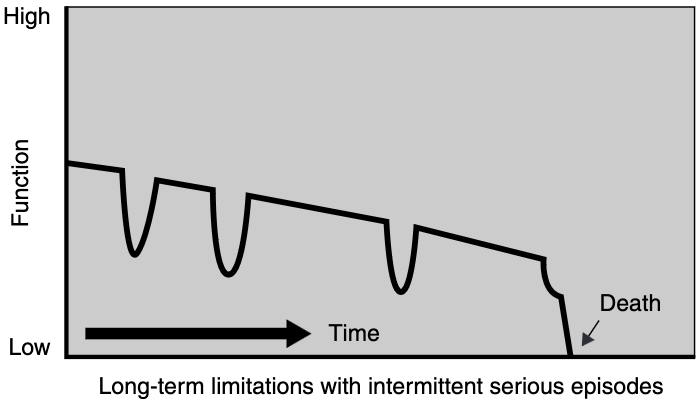
- Lynn J, Adamson DM. Living Well at the End of Life:Adapting Health Care to Serious Chronic Illness in Old Age. RAND Corporation; 2002 Dec [cited 2024 Feb 1].
- Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ. 2005 Apr 30;330(7498):1007–11.