Leukaemia
Haematological malignancy causing uncontrolled proliferation of abnormal haematopoietic progenitor cells, which:
- Replaces normal bone marrow with dysfunctional leukocytes
Leads to bone marrow failure, characterised by:- ↓ Haematopoiesis
- Immunocompromise
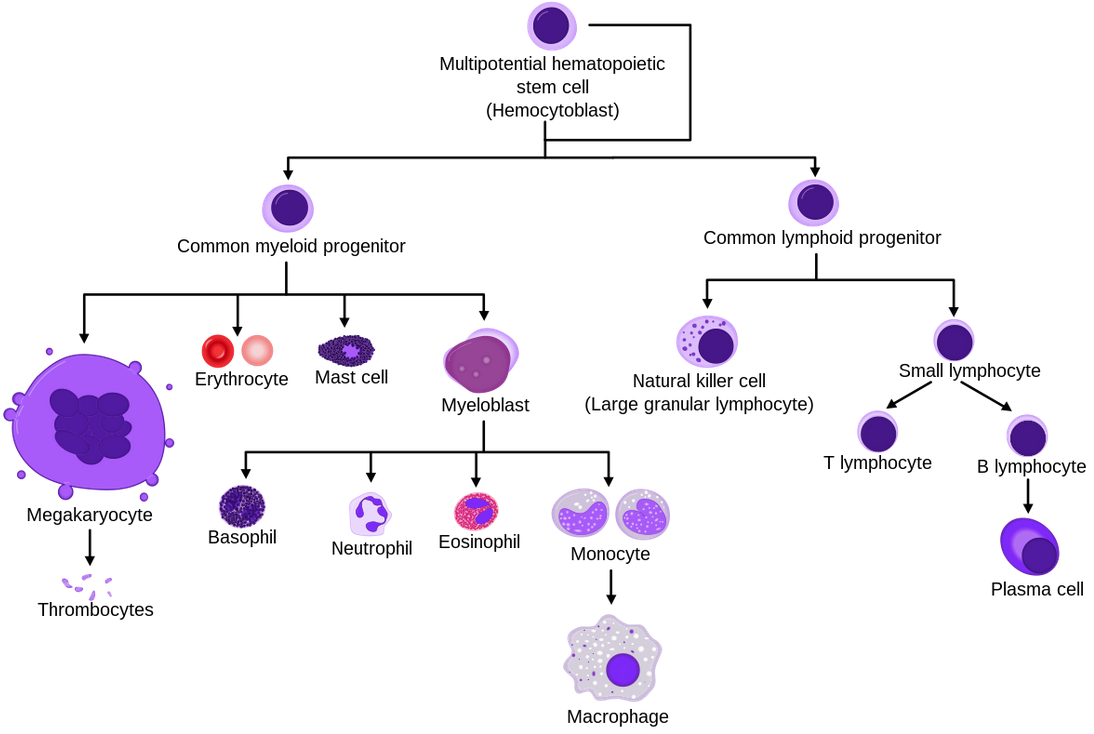
- Classified based on the type of haematological progenitor cell affected:
- Acute Myeloid Leukaemia
Uncontrolled proliferation of myeloid precursors. Rapidly progressive leukaemia which are further divided into:- AML with characteristic genetic abnormalities
Generally good prognosis. Includes:- Several known translocations
- Acute promyelocytic leukaemia (APML)
Associated with DIC.
- AML with multi-lineage dysplasia
Typically progresses from myelodysplasia and has poor prognosis. - Therapy-related AML
AML following chemotherapy or radiotherapy.
- AML with characteristic genetic abnormalities
- Acute Lymphoblastic Leukaemia
Uncontrolled proliferation of lymphoid precursors.- Usually seen in childhood
- Good prognosis
- CNS involvement is common
- Chronic Lymphocytic Leukaemia
Slow-growing accumulation of mature but abnormal lymphocytes.- Common in elderly
- 8-12 year median survival
- May transform to diffuse large B cell lymphoma
This has a very poor prognosis.
- Chronic Myeloid Leukaemia
Accumulation of mature but abnormal lymphocytes that is divided into three phases, which advance as additional mutations accrue:- Chronic phase
May last several years, with minimal symptoms. - Accelerated phase
More rapid proliferation with ↑ symptoms. - Blast crisis
Proliferation of immature blasts, resembling acute leukaemia.
- Chronic phase
- Ambiguous lineage
Evidence of either both lymphoid and myeloid cells, or where there are not enough categories to accurately classify it.
- Acute Myeloid Leukaemia
Epidemiology and Risk Factors
Pathophysiology
Aetiology
Clinical Features
Presentation typically with:
- Fatigue
- Lymphadenopathy
- Hepatosplenomegaly
- Marrow failure
- Anaemia
- Bleeding
- Immunocompromise
Assessment
History:
Exam:
Investigations
Bedside:
Laboratory:
Imaging:
Other:
Diagnostic Approach and DDx
Diagnosis confirmed with:
- Blast cells
- Immunophenotyping
- Cytogenetic analysis
- Molecular genetic analysis
Management
- Chemotherapy
Resuscitation:
Specific therapy:
- Pharmacological
- Chemotherapy
- Consists of three phases:
- Induction chemotherapy
Achieve remission by ↓ cells to undetectable levels. - Consolidation chemotherapy
Eliminate residual undetectable disease. - Maintenance therapy
Prolong remission. Used in ALL and APML.
- Induction chemotherapy
- Intrathecal chemotherapy used if CNS is involved
- Consists of three phases:
- Total body radiotherapy
- Chemotherapy
- Procedural
- Radiotherapy
- Physical
Supportive care:
Disposition:
Preventative:
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
Prognosis
Key Studies
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.