Blast Trauma
Explosions occur due to a rapid release of chemical energy and cause harm via three mechanisms:
- Primary injury
Pressure wave causing barotrauma due to over-, then under-pressurisation.- Affects air filled organs
- Risk with:
- Military trauma
Civilian primary blast trauma is rare, and associated with:- Combustion of air-dust mixtures
Coal, grain stores. - BLEVE
Gases stored as liquids under pressure explode when heating to a temperature above their boiling point.
- Combustion of air-dust mixtures
- Underwater explosions
- Explosions in enclosed spaces
- Military trauma
- Secondary injury
From projectiles propelled by the explosion.- Often penetrating injury
- Tertiary injury
From movement of air.- Often blunt trauma
- Patient being thrown into objects
- Building collapse
- Quaternary injury
Everything else:- Burns
- Toxic gases
- CO
- CN
- Oxygen depletion
- Dust
Explosions produce three key effects:
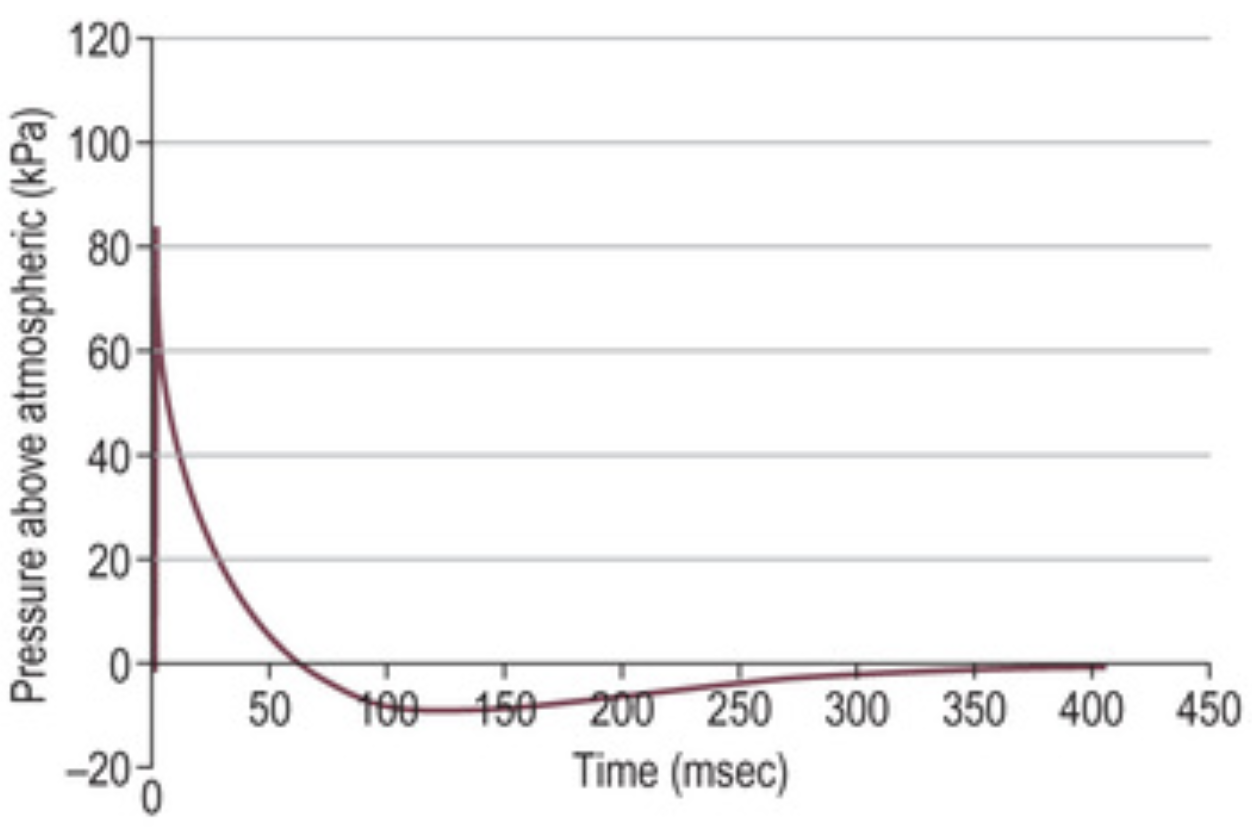
- Supersonic pressure wave
Rapid ↑ followed by ↓ of atmospheric pressure without mass particle movement.- ↑ In enclosed spaces due to reflection
- Heat
Blast wind created by gases produced during the explosion. - Gas
Epidemiology and Risk Factors
Pathophysiology
Aetiology
Clinical Features
Primary blast injury:
- Air filled organs
- Lung
- Pneumothorax
- Lung contusion
- Alveolar haemorrhage
- Blast lung
Alveolar consolidation with fluid and cellular debris.- May lead to alveolar-pulmonary venous fistuale and air embolism
- Tympanic membrane rupture
- Hollow visceral rupture
- Lung
- Globe rupture
- Mild TBI
Secondary blast injury:
- Penetrating injury
- Soft-tissue trauma
- Traumatic amputation
Tertiary blast injury:
- Blunt and penetrating injury
- TBI
- Crush injury
- Entrapment
Diagnostic Approach and DDx
Investigations
Bedside:
Laboratory:
Imaging:
Other:
Management
Resuscitation:
- A
- Intubation
- B
- Lung protective ventilation
- Minimise Pip
Risk of systemic air embolism due to direct alveolar-venous communication.
- Minimise Pip
- Lung protective ventilation
Specific therapy:
- Pharmacological
- Procedural
- Physical
Supportive care:
Disposition:
Preventative:
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
- B
- ARDS
- C
- Air embolism
- D
- Permanent hearing loss
- Tinnitus
- Abnormal vestibular function
Prognosis
Death:
- 70% occur within 5 minutes of injury due to catastrophic:
- Haemorrhage
- Brain injury
Key Studies
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.