Critical Illness Weakness
Combination of myopathy and neuropathy that occurs in the ICU patient, that is:
Formal diagnosis of CIN/CIM requires electrophysiology studies, which are rarely performed in practice and are predominantly a research tool. Criteria include:
- CIN
- ↓ AP amplitude
⩾2 nerves have amplitude <80% LLN for both:- Compound muscle
- Sensory nerve
- Normal nerve conduction velocity
- No change on repetitive stimulation
- ↓ AP amplitude
- CIM
- Preserved sensory nerve function
- ↓ Muscle excitability in ⩾2 muscle groups
- Characterised by:
- Proximal myopathy
- Symmetrical flaccid weakness
- Hyporeflexia
- Subdivided into Critical Illness:
- Myopathy
Almost universal in the critically ill, and contributes to the majority of ICU acquired weakness. - Neuropathy
Rarer than CIM. - Neuromyopathy
Combination of neuropathy and myopathy.
- Myopathy
Epidemiology and Risk Factors
Weakness is common in ICU patients:
- 65% of patients after 5-7 days of ventilation
Risk factors relate predominantly to ↓ muscle mass:
Patient factors have substantial overlap, are mutually reinforcing, and could broadly be summarised as frailty.
- Patient factors
- Age
- Low-baseline muscle mass
- Chronic disease
- Disease factors
- Severity of illness
- ICU length of stay
- Hyperglycaemia
Notably, muscle relaxants are not associated with ↑ CIM/CIN
Pathophysiology
Myopathy:
- Loss of muscle mass
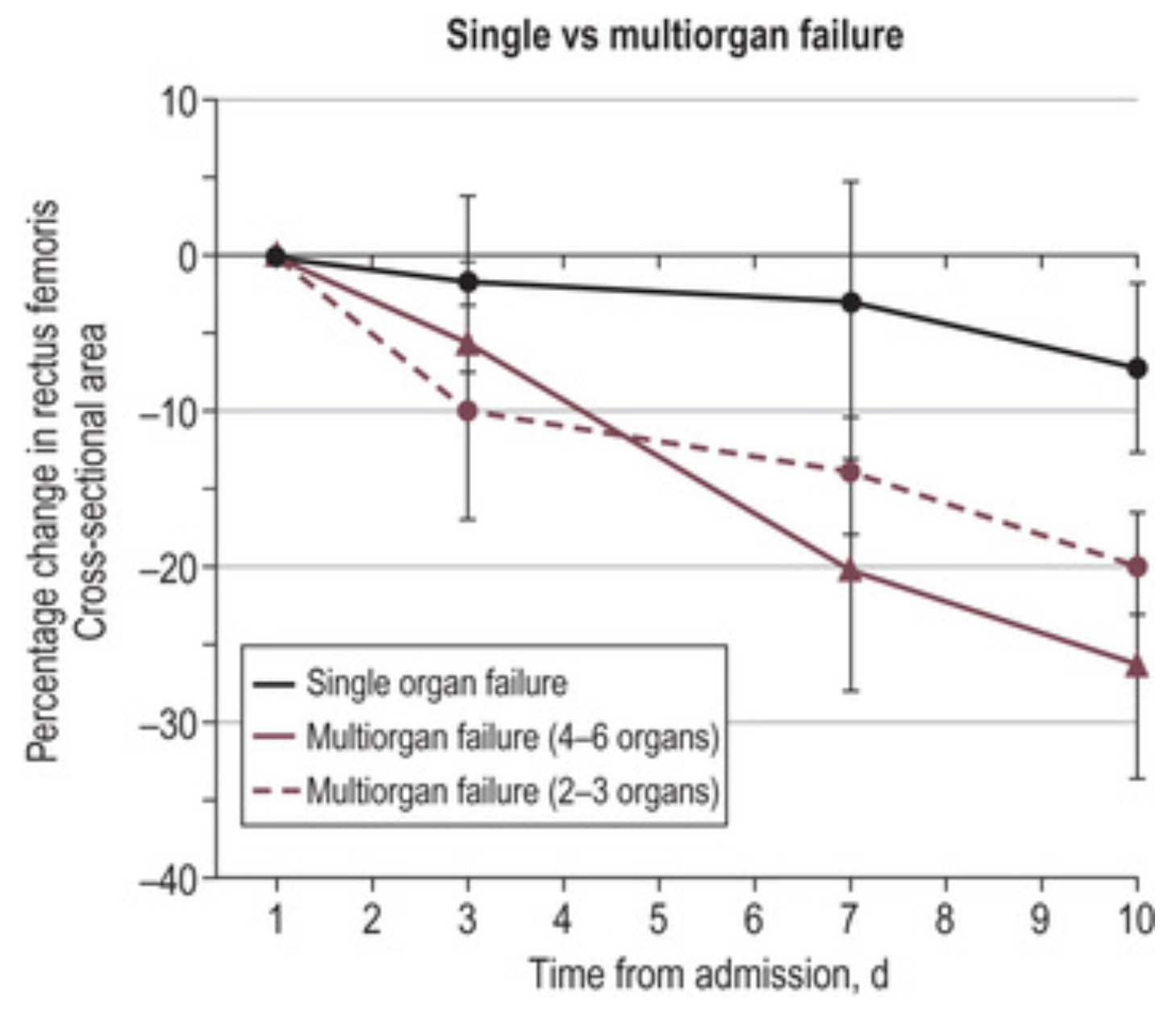
- Rapid ↓ in muscle mass within 3 days of ICU admission:
- 10% ↓ in thickness and cross-sectional area within first 3 days
- Further 10% ↓ over following 4 days
Usually 2-3%/day.
- ↑↑ Speed of wasting with ↑ number of organ failures
- Rapid ↓ in muscle mass within 3 days of ICU admission:
- ↓ Anabolism
- Altered protein metabolism
- Generalised inflammation
- Myonecrosis
- ↓ Skeletal muscle ATP synthesis
Neuropathy:
- Acquired channelopathy of voltage-gated sodium channels
Widely present but poor correlation with dysfunction. - Axonal degeneration
- Associated with ↑ BSL
Aetiology
Clinical Manifestations
Diagnostic Approach and DDx
Differential diagnoses of weakness include:
- Brainstem
- CVA
- Locked-in syndrome
- Spinal cord
- Transverse myelitis
- Mass effect
- Tumour
- Haemorrhage
- Peripheral nerve
- GBS
- CIN
- Toxins
- Arsenic
- Thallium
- NMJ
- Neuromuscular blockade
- MG
- Lambert-Eaton syndrome
- Toxins
- Organophosphate
- Botulism
- Muscle
- Steroid myopathy
- Alcoholic myopathy
- Polymyositis
- Dermatomyositis
- Toxic myopathy
- CIM
Investigations
Bedside:
Laboratory:
Imaging:
Other:
- Electrophysiology
- Rarely performed in practice
- Required for diagnosis of peripheral nerve injury
Management
Specific therapy:
- Pharmacological
- Procedural
- Physical
Supportive care:
- E
- Physiotherapy
- ↓ Catabolic effects of immobilisation and bed rest
- ↑ Anabolism
- Physiotherapy
- G
- Feeding
↑ Anabolism. - Insulin
↑ Anabolism.
- Feeding
Disposition:
Preventative:
- Minimise sedation and ventilation time
- Early wakening
- Spontaneous breathing
- Early mobilisation
Marginal and Ineffective Therapies
- Electrical stimulation
No ↑ muscle mass, possibly due to:- Impaired anabolic response
- Electrical damage to muscle
- Extra nutrition
No ↑ muscle mass or outcome improvement. - Tight glucose control
Does ↓ muscle mass loss, but results in ↑↑ hypoglycaemia and ↑ mortality.
Anaesthetic Considerations
Complications
- Death
- D
- Persistent weakness
- E
- ↑ Osteoporosis and fracture risk
Prognosis
Significant morbidity and mortality:
- Mortality
↑ Short-term and 5-year mortality. - Morbidity
Severe functional limitations occur among survivors:- At 6-12 months
- 70% have substantial limitations
- 30% are carer-dependent
- At 6-12 months
Key Studies
References
- Nakanishi N, Oto J, Tsutsumi R, Iuchi M, Onodera M, Nishimura M. Upper and lower limb muscle atrophy in critically ill patients: an observational ultrasonography study. Intensive Care Med. 2018 Feb;44(2):263-264.
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.