Chronic Obstructive Pulmonary Disease
COPD is a chronic, progressive inflammatory disease characterised by persistent respiratory symptoms with incompletely reversible airflow limitation. COPD:
- Affects airways, lung parenchyma, and vasculature
- Impairs expiration via:
- Poorly reversible airway narrowing
- Airway smooth muscle remodelling
- ↑ mucous production
- Includes bullous disease
Epidemiology and Risk Factors
Common comorbidity:
- 10% of >40s worldwide
- 4th most common cause of death
- Associated with:
- CAD
- Malignancy
- Depression
Risk factors:
- Environmental exposures:
- Smoking
- Cigarettes
- Pipes/cigars
- Water pipe
- Marijuana
Greater ↑ in bullous emphysema due to holding hot inhaled smoke.
- Occupational exposures
- Dusts
- Chemical agents
- Fumes
- Indoor air pollution
- Cooking fuels
- Outdoor air pollution
Relatively small effect.
- Smoking
- Genetic factors:
- FAM13A associated with development
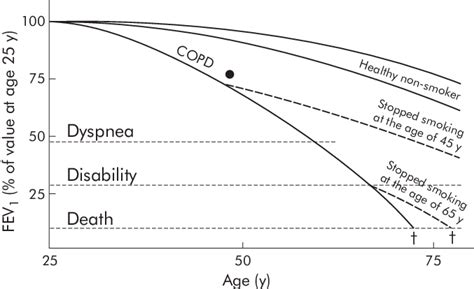
Degree of decline in FEV1 with age varies with the duration of smoking, timing of quitting smoking, and susceptibility to COPD.
Pathophysiology
Expiratory airflow limitation via:
- ↑ Airway resistance:
- Obstructive bronchiolitis
Small airway inflammation leads to gas trapping and dynamic hyperinflation. - ↑ Secretion production
- Bronchospasm
- Parenchymal destruction
Leading to emphysema, which reduces:- Pulmonary capillary bed volume
- Lung surface area for gas exchange
- V/Q matching
- Obstructive bronchiolitis
- Loss of elastic recoil
Combination of elastin destruction and fall in alveolar surface tension.- ↓ Expiratory air flow
Air flow limitation leads to:
- Prolonged expiration
- Pulmonary hyperinflation
- ↑ work of breathing
- Dyspnoea
Aetiology
Assessment
Key symptoms are:
- Chronic cough or sputum production
- History of exposures
- Dyspnoea
Graded using the mMRC scale.
| MRC Grade | Breathlessness |
|---|---|
| Grade 0 | Only with strenuous exercise |
| Grade 1 | Hurrying or a slight incline |
| Grade 2 | Slower than people of same age; stopping due to shortness of breath on flat ground |
| Grade 3 | After ~100m or a few minutes on flat ground |
| Grade 4 | Too breathless to leave the house; breathless when dressing/undressing |
GOLD Criteria
Global Initiative for Obstructive Lung Disease Criteria:
- Used clinically to determine severity of disease in order to prognosticate and guide therapeutic interventions
- Not appropriate for diagnosis
- Are based upon:
- Symptom burden
mMRC score. - Number of exacerbations and hospital admissions
- FEV1
- Symptom burden
Treatment recommendations:
- GOLD A
Bronchodilator (LABA or SABA) offered, and continued if effective. - GOLD B
LABA or long-acting methacholine antagonist should be offered as initial therapy. - GOLD C
LAMA as initial therapy, and benefit may be seen with LAMA & LABA & inhaled corticosteroids. - GOLD D
LAMA & LABA as initial therapy, with inhaled corticosteroids for patients with frequent exacerbations.
Diagnostic Approach and DDx
Diagnosis should be considered in:
- Smokers
- Age >35
- Exertional breathlessness
- Chronic cough
- Frequent winter bronchitis or wheeze
Differentials include:
- Chronic asthma
Long-term dyspnoea from childhood, with obvious precipitants. Normal TLCO with reversibility. - Late-onset asthma
Associated with GORD. Normal TLCO with reversibility. - Broncholitis obliterans
Investigations
Laboratory:
- Bloods
- α-1 antitrypsin
All patients should be screened once for α1 antitrypsin deficiency. ⩽20% is suggestive of homozygous deficiency. - ABG/VBG
Evaluate degree of chronic hypercapnoea and metabolic compensation.
- α-1 antitrypsin
Imaging:
- CXR
Hyperinflation if >=10 posterior ribs visible.
Other:
- Respiratory Function Tests
- Diagnostic
- Used to grade severity:
- FEV1FVC/ of ⩽0.7
- Reversibility is not required
Differentiated from asthma on clinical grounds.
- Reversibility is not required
- Severity graded by FEV1
Multiple grading systems, the GOLD 2008/NICE 2010 system:- FEV1 ⩾80% predicted
Mild. - FEV1 50-79% predicted
Moderate. - FEV1 30-49% predicted
Severe. - FEV1 ⩽30% predicted
Very severe.
- FEV1 ⩾80% predicted
- FEV1FVC/ of ⩽0.7
Management
Specific therapy:
- Pharmacological:
- Inhaled therapies
Mainstay of day-to-day treatment. Includes: * Short-acting bronchodilators
For breathlessness and exercise limitation. * Long-acting bronchodilators
For persistent breathlessness.- Oral therapy
Regular oral corticosteroids may be requried in advanced disease. - Vaccination
Influenza and pneumococcal vaccines ↓ LRTI rate.
- Oral therapy
- Inhaled therapies
- Procedural
- Lung volume reduction surgery
Improves survival in severe upper-lobe emphysema and low post-rehabilitation exercise capacity. - Bullectomy
Improves dyspnoea, lung function, and exercise tolerance is selected patients. - Lung transplantation
Improves quality of life in selected patients with very severe COAD. - Bronchoscopic interventions
Includes coils and endobronchial valves, and improves exercise tolerance and lung function at 6-12 months following treatment.
- Lung volume reduction surgery
- Physical
- Smoking cessation
Vital, and will slow down deterioration and disability before death occurs. - NIV
Reduces chronic hypercarbia, survival, and readmission rates. - Home oxygen
Indicated in patients with severe resting hypoxia (PaO2 <60mmHg, or ⩽55mmHg with cor pulmonale or pulmonary hypertension).
- Smoking cessation
Acute Exacerbation of COPD
Acute change in degree of dyspnoea, cough, or sputum production. Acute exacerbations are:
- The most common admission diagnosis in the UK (~16%)
- Usually survivable in the short term but a poor prognostic sign for survival in the medium-long term
Up to 90% hospital survival, but significantly impaired 2-3 year survival.
Common precipitants:
- Infection
- Most commonly bacterial:
80% caused by:- S. Pneumoniae
- H. Influenze
- Viral isolated in 20-30%:
- Rhinovirus
- Influenze
- Parainfluenzae
- Most commonly bacterial:
- Sputum retention
- Cardiac failure
- Other respiratory disease
- Pneumothorax
- Uncontrolled oxygen therapy
Relative hyperoxia (>92%) may adversely affect V/Q matching, reduce hypoxic drive, and ↑ CO2 dissociation via the Haldane effect.
Specific therapy:
- Physical
- Oxygen
Target SpO2 88-92%. - HFNO
- NIV
Preferred over invasive ventilation, and indicated when:- Uncompensated respiratory acidosis
- Severe dyspnoea with signs of fatigue
- Persistent hypoxaemia despite supplemental oxygen
- Chest physio
- Encourage coughing
- Bubble PEEP
- Invasive ventilation
Reasonable in patients without end-stage lung disease - 80-90% wean successfully. Avoid breath stacking.- Suggested initial settings to avoid breath stacking
- PEEP 3-8cmH2O
- Psup 8-15cmH2O
- RR <14
Aim MV <115mL/kg.
- Minimise dynamic hyperinflation by:
- Watching the flow-volume loop
- Measuring end-inspiratory pause
Target <25cmH2O. flow-volume loop to minimise dynamic hyperinflation
- Suggested initial settings to avoid breath stacking
- Oxygen
- Pharmacological:
- Bronchodilators
Many patients have a small response, and this assists in sputum clearance.- Ipratropium 500ug Q2H
Anticholinergic agents have a greater effect compared to beta-agonists. - Salbutamol 5mg Q2H
- Ipratropium 500ug Q2H
- Steroids
Prednisolone 0.5mg/kg (or equivalent) for 5 days. - Antibiotics
Amoxycillin usually first line for S. pneumoniae and H. influenzae cover. - Electrolyte correction
- DVT prophylaxis
- Bronchodilators
Anaesthetic Considerations
- B
- Smoking cessation
Patients are more receptive to smoking cessation perioperatively, and this should be encouraged. - Disease severity
- Exercise tolerance
- Number of exacerbations
- Most recent course of antibiotics or steroids
- Previous requirement for NIV or intubation
- Wheezing
If present needs aggressive treatment with bronchodilators +/- steroids. - Active respiratory infection
Consider treatment and postponing surgery. - Consider CXR if:
- Current infection
- Recent deterioration in symptoms
- Ventilator settings
Aim to minimise gas trapping:- ↑ the I:E ratio to prolong expiratory time
Suggest 1:3-1:5.- May require ↑ inspiratory flow rate and higher Pip
- Consider PEEP
Aim to splint open small airways, and if ePEEP < iPEEP then worsening of CV effects will not occur. - Bronchospasm
- ↑ the I:E ratio to prolong expiratory time
- Smoking cessation
- C
- Pulmonary hypertension
- Concomitant IHD
- D
- General anaesthesia
↑ Risk, particularly with intubation and IPPV, of:- Laryngospasm
- Bronchospasm
- Barotrauma
- Hypoxaemia
- Cardiovascular instability
- Regional anaesthesia
- General anaesthesia
- E
- Neuromuscular blockade
- Ensure complete reversal prior to extubation
- Consider extubation directly onto NIV
Reduces need for post-operative reintubation.
- Neuromuscular blockade
Marginal and Ineffective Therapies
Complications
- Death:
- 8% in-hospital mortality
- 15% 90-day mortality
- Up to 50% 1-year mortality
- B
- Recurrent infection
↑ With Pseudomonas colonisation
- Recurrent infection
Prognosis
- Lung cancer is frequently seen and is the major cause of death
Key Studies
References
- Lumb A, Biercamp C. Chronic obstructive pulmonary disease and anaesthesia. Contin Educ Anaesth Crit Care Pain. 2014 Feb 1;14(1):1–5.
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.