Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome
HIV is a retrovirus that infects immune cells, leading to:
- An initial, non-specific viral infection
Termed seroconversion illness. - Chronic immunodeficiency
Termed AIDS.
When it was first identified, HIV was named HTLV-3 (Human T-lymphotropic Virus), and the more common (and pathogenic) variant named HIV-1 after the rarer and less virulent HIV-2 was discovered in West Africa.
Epidemiology and Risk Factors
Pathophysiology
Viral exposure results in:
- Initial infection of cell surface receptor
Classically CD4, though other receptors are implicated as co-receptors.- Viral RNA is integrated into cellular DNA
- RNA transcribed from cellular RNA, and translated into viral protein
- Initial viraemia presents as seroconversion illness, and is typically controlled by initial immune response
- HIV replication continues in a largely asymptomatic fashion
- Progressive immune deficiency occurs despite persistent host immune response, with ↓ in CD4+ T cells
Rate varies depending on host and viral factors:- Median ~9 years
- Some show no evidence of CD4 loss for up to 15 years
Aetiology
Clinical Manifestations
Seroconversion illness occurs 1-4 weeks following exposure:
- Fever
- Lymphadenopathy
- Headache
- Photophobia
- Fatigue
Chronic infection may cause:
- Fever
- Weight loss
- Lymphadenopathy
- Diarrhoea
Diagnostic Approach and DDx
Investigations
Bedside:
Laboratory:
- Bloods
- Diagnosis
- anti-HIV antibodies
Diagnostic of infection; positive in most patients within 3 months of infection.
- anti-HIV antibodies
- Monitoring
3-4 monthly testing in stable patients.- HIV viral load
- CD4+ count
- Best indicator of severity of immunodeficiency and susceptibility to infection
- AIDS-related illnesses unlikely if >200
- Diagnosis
Imaging:
Other:
Management
Resuscitation:
ABC approach. Comment on team coordination and clinical priorities.
Specific therapy:
- Pharmacological
- Antiretroviral therapy
Each drug acts at different points in the replication cycle, and so combination therapy is essential.- Triple combination therapy usually leads to sustained control without resistance development
- Initiation by HIV specialist
- Potential significant drug interactions
- Timing of therapy in the setting of infection is controversial
In general:- Delay initiation until 2-4 weeks after treatment of aids defining illness
Longer in more severe disease with ↑ risk of Immune Reconstitution Inflammatory Syndrome.
- Delay initiation until 2-4 weeks after treatment of aids defining illness
- Antiretroviral therapy
- Procedural
- Physical
Significant drug interactions may occur with:
- Anaesthetics
- Midazolam
- Antimicrobials
- Antiemetics
- Anticonvulsants
- Anticoagulants
- Statins
Supportive care:
Disposition:
Preventative:
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
Divided into:
Pulmonary infections are more common at higher CD4 counts, extra-pulmonary infection becomes more common as CD4 counts fall.
- Direct complications of immune deficiency
- Infections
- Immunocompromised
- PJP
- Oesophageal candidiasis
Common presenting disease. - Cryptococcal meningitis
Non-specific and not-particularly-meningitic presentation:- Headache
- Fevers
- Minimal neck stiffness
Relies on inflammation of the meninges, which in turn relies on a functioning immune response.
- Mycobacterium avium complex
- CMV retinitis
- TB
- Cerebral toxoplasmosis
- Focal encephalitis
- Requires brain biopsy for diagnosis
- Generic
- Sepsis
- Pneumonia
- Immunocompromised
- Tumours
- Immunocompromised
- T-cell lymphoma
Particularly CNS lymphomas. - Karposi Sarcoma
Angioproliferative tumour of epithelium relating to herpes virus 8 infection, which presents as red-purple lesions on skin and oral and gastric mucosa.
- T-cell lymphoma
- Immunocompromised
- Immune reconstitution syndrome
- Infections
- Indirect complications
- C
- Autoimmune vasculitis
- Dilated cardiomyopathy
- CAD
- D
- Autonomic neuropathy
- Drug-related
- Type B lactic acidosis
- Pancreatitis
- AKI
- Stevens-Johnson syndrome
- C
Prognosis
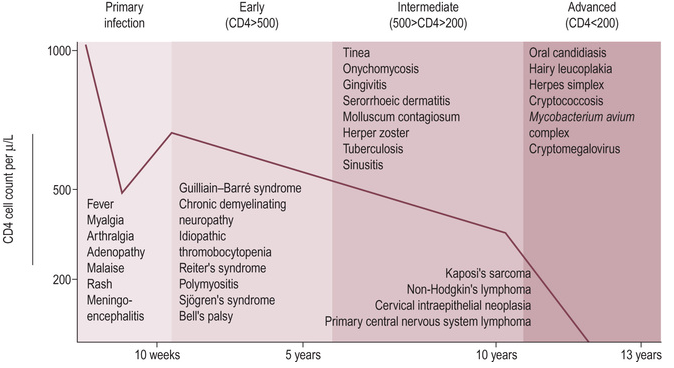
The natural history of HIV is a general decline in immune function with an ↑ burden of exotic and severe disease:
With access to antiretroviral therapy, mortality approaches that of the general population.
Key Studies
References
- Nelson, Ann Marie, Yukari C. Manabe, and Sebastian B. Lucas. “Immune Reconstitution Inflammatory Syndrome (IRIS): What Pathologists Should Know.” Seminars in Diagnostic Pathology, Seminars Issue on HIV-related Disease, 34, no. 4 (July 1, 2017): 340–51. .
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.