Proning
Proning is a treatment for refractory hypoxaemia in T1RF that:
Proning is a cornerstone of ARDS management. ARDS is covered in detail under Acute Respiratory Distress Syndrome.
- Promotes homogenous lung ventilation
Creates a more uniform distribution of pleural pressure, which:- ↓ Cyclical atelectasis and atelectotrauma
- Improves V/Q mismatch
- ↓ Lung deformation
Relieves compression of the lungs from the mediastinum and abdominal contents. - ↑ FRC
- Facilitates secretion drainage
- Reverses hypoxia due to shunt
Indications
Indicated with:
- Appropriate expertise
- Severe hypoxaemia (P/F <150) in lung pathologies that are:
- Diffuse
- Acute
- Reversible
- Dorsal wounds
- Burns
- Surgical wounds
Contraindications
Prone position is contraindicated in patients with risk of:
- Turning
- C-spine injury
- Unstable T/L spine
- Unstable pelvis
- Being supine
- Facial trauma
- Open chest
- Open abdomen
- Pregnancy
- Intraabdominal hypertension
- Ventral wounds
Principles
Proning is effective as:
- Lung parenchymal volume is larger posteriorly than anteriorly
- There is greater V/Q mismatch to posterior regions when supine due to:
- Atelectasis and collapse
- Dependent oedema
- ↑ Pulmonary blood flow
- Prone ventilation
- Recruits collapsed regions
- ↑ Secretion drainage
Practice
- Consider prone ventilation early and often
- 16 hours
- 5 days or until no further response required
- Adjunct to lung protective ventilation and VV ECMO
- Timing of proning and de-proning should occur with experience staff present to manage any complications
Complications
- A
- Airway loss
- Sputum plugging
- C
- Dislodgement of lines and devices
- D
- Blindness
- Ocular pressure injury
- ↓ Retinal perfusion pressure
- Blindness
- E
- Pressure areas
Key Studies
- PROSEVA (2013)
- 474 Europeans with ARDS (PF <150mmHg), intubated for <36 hours at inclusion
- Multicentre (experienced proning units), assessor-blinded, RCT
- 456 patients gives 90% power for 15% ARR from control mortality of 60%
- Randomised to proning vs. supine
- Proning
16 consecutive hours for 28 days, or until improvement. - Standardised ventilation and weaning strategy
- Proning
- Significant ↓ mortality (16% vs. 33%, OR 0.42 (0.26-0.66), NNT 6) in proning group
- Over 2000 patients were not screened
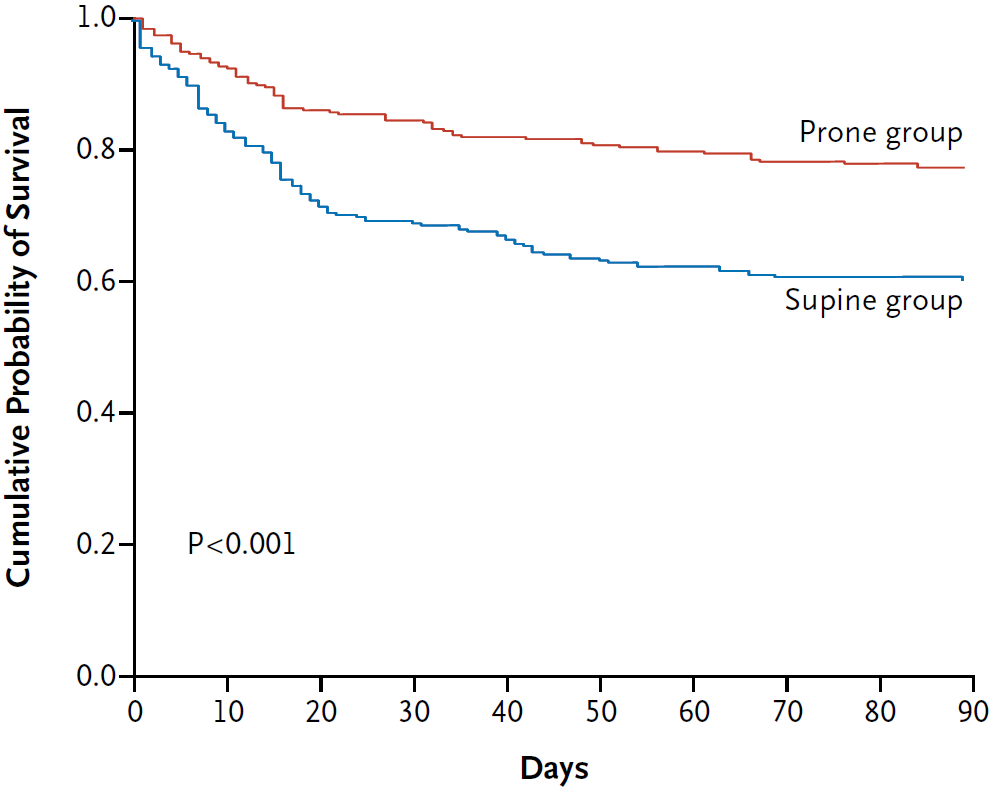
PROSEVA was the definitive trial on proning.
References
- Guérin C, Reignier J, Richard JC, et al. Prone Positioning in Severe Acute Respiratory Distress Syndrome. N Engl J Med. 2013;368(23):2159-2168. doi:10.1056/NEJMoa1214103