Diffuse Alveolar Haemorrhage
Potentially life-threatening hypoxaemic respiratory failure characterised by:
- Haemoptysis
- Anaemia
- Diffuse alveolar infiltrates
Epidemiology and Risk Factors
Pathophysiology
Aetiology
Precipitants include:
- Pulmonary capillaritis secondary to autoimmune disease, including:
- Systemic vasculitis
- Granulomatosis with Polyangiitis
- Churg-Strauss syndrome
- Microscopic polyangiitis
- Primary immune complex-mediated vasculitis
- Goodpasture’s syndrome
- Henoch-Schonlein purpura
- Secondary vasculitis
- SLE
- RA
- APS
- Mixed connective tissue disease
- POlymyositis
- Dermatomyositis
- Essential cryoglobulinaemia
- Behcet’s disease
- Anti-GBM disease
- Systemic vasculitis
- Coagulation disorders
- Pulmonary vascular disease
- MS
- Pulmonary veno-occulisive disease
- Drugs
- Amiodarone
- Nitrofurantoin
- Chemotherapeutics
- Propylthiouracil
- Toxins
- Transplantation
- BMT
- ARDS
Assessment
Presentation typically with:
- Fever
- Dyspnoea
- Cough
Haemoptysis is rare. - Blood alveolar lavage samples
History
Exam
Investigations
Bedside:
Laboratory:
A rheumatological screen consists of:
- Initial investigations:
- FBE
- UEC
- ESR
- CRP
- LFT
- ANA
- Rheumatoid factor
- Anti-CCP antibodies
- Vitamin D
- Urinealysis
- Second-line investigations
For patients with strong clinical suspicion:- Anti-synthetase antibodies
- Creatine kinase
- Aldolase
- Sjögren’s antibodies
- SS-A
- SS-B
- Scleroderma antibodies
- Anti-topoisomerase (Scl-70)
- Anti-PM-1 antibody
- Anti-centromere
- Anti-dsDNA antibodies
- Myositis-associated antibodies
- Jo-1
- PL-7
- PL-12
- ANCA
- Anti-melanoma differentiation-associated gene 5
- Overlap antibodies
PM-1.
- Blood
- FBE
- Coagulation screen
- Rheumatoid screen
Imaging:
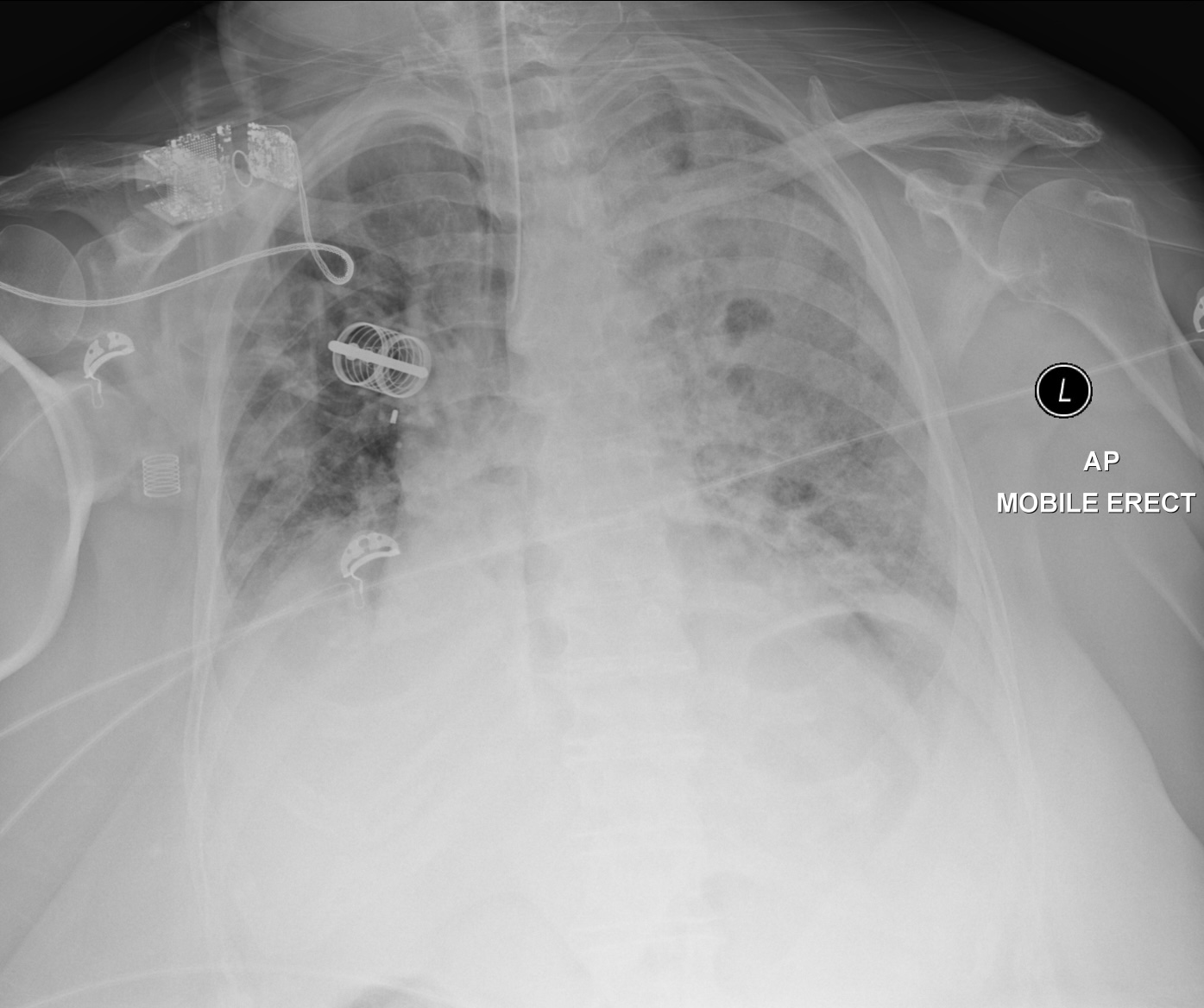
- CXR
- High-resolution CT Chest
Other:
- BAL
Essential for diagnosis, and to exclude infection.
Diagnostic Approach and DDx
Management
- Treat underlying cause
- Immunosuppression
Corticosteroids as first line therapy.
Resuscitation:
- A
- Intubation and mechanical ventilation
Specific therapy:
- Pharmacological
- Corticosteroids
- Methylprednisolone 500mg Q6H for 4-5 days, followed by taper
- Other immunosuppressants may be indicated
- Methotrexate
- MMF
- Etanercept
- Corticosteroids
- Procedural
- Plasmapheresis
If indicated for the primary immunological precipitant, e.g. Goodpasture’s or vasculitis.
- Plasmapheresis
- Physical
Supportive care:
Disposition:
Preventative:
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
- Death
Prognosis
Key Studies
References
- Park MS. Diffuse Alveolar Hemorrhage. Tuberc Respir Dis (Seoul). 2013 Apr;74(4):151–62.
- Case courtesy of Jan Frank Gerstenmaier. Radiopaedia.org. From the case: rID: 28582.