Cardiac Advanced Life Support
This section covers the algorithmic management of cardiac arrest in an adult patient who is up to 14 days after cardiac surgery.
Key differences from standard ALS include:
- Environment
Patients often:- In the ICU
- Invasively monitored
- Have epicardial pacing wires
- Therapy
- If VF/VT Reasonable to delay CPR for 1 minute to facilitate cardioversion
- If asystole: pace DOO 100 at maximal amplitude
- If PEA: Turn off pacing (exclude VF)
Epidemiology
Cardiac arrest post cardiac-surgery:
- Occurs in 1-5%
- 50% within 3 hours of ICU admission
- Majority within 24 hours
Protocol
This algorithm assumes that the patient has ECG and invasive arterial monitoring:
- Recognition
Arrest is consistent with:- Loss of central pulse
- Loss of all invasive pressures
- Systemic arterial pressure
- Pulmonary arterial pressure
- CVP
- Pulse oximetry
- Loss of ETCO2
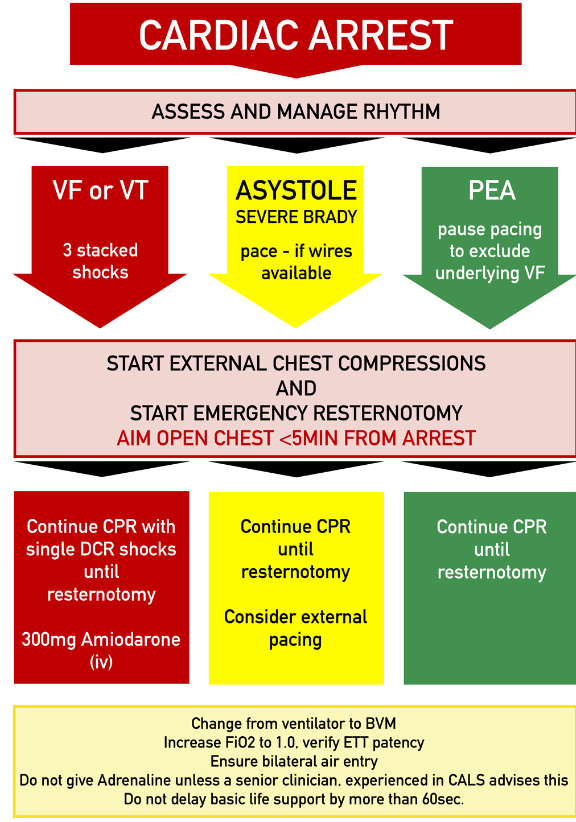
- Assess rhythm
- VF/VT
- DC shock
Up to 3 attempts. - Amiodarone
300mg. Further loading of 150mg followed by infusion may be given for refractory VT/VF
- DC shock
- Asystole/Severe bradycardia
- Pace
In DDD or DOO at 100bpm and at maximal amplitude.
- Consider external pacing
- Pace
- PEA
- Pause pacing to exclude underlying VF
- VF/VT
- Start BLS
External Cardiac Compressions:- May be delayed up to 1 minute to facilitate cardioversion, with the goal of ↓ trauma from chest compressions
- Standard site, depth, and compression ratio
- An SBP of >60mmHg should be targeted if invasive arterial monitoring is present
- Inability to achieve an SBP of >60mmHg with compressions indicates need for immediate resternotomy
- Prepare for emergency resternotomy
Chest should be opened within 5 minutes of arrest.
Delay of chest compressions is appropriate to minimise iatrogenic trauma, and in recognition that it is minimally effective in obstructive and hypovolaemic causes of shock.
Adjuvant management:
- Airway
- Change to BVM with 100% O2
- Breathing
- PEEP to 0cmH2O
Improve cardiac preload in the setting of tamponade/hypovolaemia.- Consider ↑ PEEP if arrest secondary to hypoxia
- Auscultate/ultrasound to evaluate for tension pneumo/haemothorax
Decompress if present.
- PEEP to 0cmH2O
- Circulation
- Avoid adrenaline unless advised by senior clinician
Typical dose is 50-300ug. - Give fluid bolus
- Activate massive transfusion
- Pause infusions
- Evaluate for dosing/drug errors
- Consider restarting vasopressor infusions
- Lignocaine 1mg/kg may be considered as an alternative to amiodarone
- Change IABP settings:
- Pressure trigger
- Maximum augmentation
- 1:1 ratio
- Consider echocardiography
Use should not delay CPR or resternotomy.
- Avoid adrenaline unless advised by senior clinician
Emergency Resternotomy
Resternotomy occurring ⩽10 minutes is associated with ~50% survival, compared to ~10% if >10 minutes
Integral part of arrest management, that should be:
- Performed in all patients within 10 days of their last operation
- Considered in patients up to 14 days after cardiac surgery
- Prepared for immediately upon identification of cardiac arrest
- Completed within 5 minutes of arrest
Indications
- Failure to achieve ROSC with above measures
- Immediately if SBP <60mmHg despite external chest compressions
Equipment
Required:
- Scalpel
- Wire cutter
- Sternal wire holder
- Suction
- Sternal retractor
e.g. Finochietto.
Optional:
- Dissection scissors
- Non-toothed forceps
Roles
Six key roles (with ⩾7 staff):
- Team leader
- ICU coordinator/scribe
- Resternotomy team
- Doctor
- Nurse
- Resternotomy trolley
Scout. - Defibrillator/pacing
- Airway/breathing
Process
- Cease chest compressions
- Remove sternotomy dressing
- Apply adhesive surgical drape without prior skin preparation
Sterile chest compressions can occur at this time whilst equipment is assembled. - Open sternotomy incision:
- Deep incision through sternotomy sutures down to sternal wires with scalpel
- Cut sternal wires with wire cutter
- Remove sternal wires with wire holder
- Clear blood and clot
- Open sternum with sternal retractor
- Open pericardium if closed
- If no output despite opening sternum:
- Consider internal defibrillation 20J with internal paddles.
- Commence internal cardiac massage
- Avoid grafts
- Right hand over apex and around behind the heart
- Left hand over anterior surface of heart
- Squeeze both hands together with flat palms and straight fingers
Aim SBP >60mmHg at a 100 bpm.
Post-procedural care:
- Transfer to OT
- Washout
- Consider closure
- Antibiotics
- Avoid fever
Temperature ⩽36°C.
References
- Society of Thoracic Surgeons Task Force on Resuscitation After Cardiac Surgery. The Society of Thoracic Surgeons Expert Consensus for the Resuscitation of Patients Who Arrest After Cardiac Surgery. Ann Thorac Surg. 2017 Mar;103(3):1005-1020.
- Truhlar A, Deakin CD, Soar J et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 4. Cardiac arrest in special circumstances. Resuscitation 2015; 95: 148-201.
- Karcher C. et al. The Australasian ANZSCTS/ANZICS Guidelines on Cardiothoracic Advanced Life Support (CALS-ANZ). Critical Care and Resuscitation 24, no. 3 (6 September 2022): 218–23.