Neuroprognostication
This is an overview of neuroprognostication. It is generally tailored to cardiac arrest, although there is substantial overlap with TBI prognostication.
Accurate prediction of neurological outcome is difficult and critical:
- Neurological outcome is a major determinant of quality of life and ongoing healthcare needs
- Overly pessimistic prognosis leads to withdrawal of life sustaining therapy in patients who could potentially recover
- Overly optimistic views lead to prolongation of support in patients with futile prognosis
Consequential ↑ healthcare-associated suffering:- Individual loss of dignity
- Invasiveness of intensive care
- Familial exhaustion
Outcome Assessment
Scales used to assess neurological outcome include:
The definition of a good outcome changed circa 2006; studies older than this typically include severe disability as a good outcome.
- Glasgow Outcome Scale
Largely deprecated. - Glasgow Outcome Scale - Extended
- Cerebral Performance Categories
Derived from the Glasgow Outcome Score, and used after cardiac arrest.- Typically, a good outcome includes moderate or minor disability (CPC 1-2)
Glasgow Outcome Scale - Extended
The Glasgow Outcome Scale - Extended (GOS-E) is commonly used to measure TBI outcome:
- Death
- Vegetative state
Unaware, periods of spontaneous eye opening, persistent reflex responses. - Lower severe disability
Dependent, unable to be left alone for >8 hours. - Upper severe disability
Dependent, able to be left alone for >8 hours. - Lower moderate disability
Independent at home, dependent outside, unable to return to work. - Upper moderate disability
Independent at home, dependent outside, able to return to work with special arrangement. - Lower good recovery
Some disability but able to return to work. - Upper good recovery
Some deficits but not disabling.
Cerebral Performance Categories
| CPC | GOS | Disability | Conscious | Independent | Features |
|---|---|---|---|---|---|
| 1 | 5 | No, or minor | Yes | Yes | Can work and lead a normal life. May have:
|
| 2 | 4 | Moderate | Yes | Yes | Can travel by public transport, work in sheltered environment, and is iADLs. May have:
|
| 3 | 3 | Severe | Yes | No | Locked-in, minimially conscious, or severe dementia. Requiring institutional care or full-time home care. |
| 4 | 2 | Unconscious | No | No | Persistent vegetative state |
| 5 | 1 | Dead | Brain or cardiac death |
Clinical Examination
Clinical examination is interfered with by hypothermia, sedation, analgesics, and muscle relaxants.
Relevant features of the neurological exam include:
- Cranial nerve findings
- Pupillary reflexes
- Corneal reflexes
- Motor score
- Myoclonus
- Status myoclonus involves synchronised, repetitive, symmetric, persistent (>30 minutes) jerking with clinical coma
- EEG may show status or general malignant pattern
- Specific for poor neurological outcome
- Status myoclonus involves synchronised, repetitive, symmetric, persistent (>30 minutes) jerking with clinical coma
| Finding | Pupillary Reflexes | Corneal Reflexes | Motor Score |
|---|---|---|---|
| <24 hours |
|
||
| 72-96 hours | Absent any is ~99% specific for poor outcome | Absent any is ~95% specific for poor outcome |
|
| >96 hours | Bilateral absence ~100% specific for poor outcome | Absent any is ~100% specific | As 72 hours. |
| Comments | Generally very insensitive (~20%) but highly specific. | Marginally more sensitive than pupillary (~30%) but less specific. |
Investigations
Laboratory:
- Bloods
- Neuron Specific Enolase
- Serial measurements demonstrating repeated and ↑ levels predict poor outcome
- Confounded by haemolysis and neuroendocrine tumours
- Unclear prognostic value
- Neuron Specific Enolase
Imaging:
Functional investigations (neurological exam, SSEPs, EEG) are generally superior to radiology at predicting outcome but more affected by confounding.
In general, radiological tests are more useful for diagnosis than prognostication.
- CT Brain
- Logistically easier than MRI
- Can be performed earlier and repeatedly
Features ↑ over 3-5 days as oedema evolves. - Features of HIE include:
- Loss of grey/white differentiation
Cytotoxic oedema ↓ grey matter density. - Diffuse oedema
- Effacement of ventricles and sulci
- Herniation
- Tonsillar
- Trans-tentorial
- Pseudo-subarachnoid haemorrhage pattern
↑ Density of basal cisterns due to ↑↑ ICP, usually occurring with generalised oedema.
- Loss of grey/white differentiation
- MRI Brain
- Prognostically useful if no HIE on CT brain
- Optimal time is 2-7 days after arrest
- Features include:
- Early: ↑ DWI intensity and diffusion restriction
- Presence is highly specific for a poor outcome
- Absence of DWI lesions is reasonably specific for a good 6-month functional outcome
- Changes may pseudonormalise at 7 days
- Late: ↑ T2/FLAIR intensity
- Early: ↑ DWI intensity and diffusion restriction
Other:
EEG and SSEP are covered in detail under Electroencephalogram and Evoked Potentials.
- EEG
- Most useful 24 hours after cardiac arrest
- Generally falsely improve over time, ↓ diagnostic utility
- Sedatives should be withheld for several half-lives prior to obtaining recording
- SSEP
- Most useful 24 hours after arrest in patients with an abnormal EEG
- Retains accuracy under sedation
- Contraindicated by cervical spine abnormality
- ↓ Accuracy after TBI due to presence of spinal or subcortical lesion
Approach
- The best predictor of future improvement is past improvement
- Earlier (hours) improvement is better than late (days) improvement
Neuroprognostication is difficult, and:
- Relies on a combination of:
- Clinical examination findings
- Structural investigations
- Functional investigations
- Becomes more accurate with time
Approach is correspondingly split into:- Early
<72 hours. Management is supportive unless unequivocal evidence of dismal outcome. - Late
- Indeterminate
- Early
Early
- Minimise confounders
- Obtain prognostic information
Principles:
- Supportive intensive care
- Avoid assessment in the setting of hypothermia
e.g. Post-arrest TTM. - Early family meeting to set expectations around:
- Time required for prognostication
- Likelihood of significant brain injury
- Gain prognostic information
- CT
- MRI
- EEG
Ideally at 12, 24, 48 hours.
Early prognostication by may be possible if there is:
- Brain death
- Unequivocal evidence of catastrophic brain injury
- Localisation or withdrawal
Favours good prognosis.
Late
- Exclude confounders
- Evaluate predictors of good and poor outcome
- Decisions guided by family input around patients wishes and acceptable quality of life
Principles:
- Rule out confounders
- Drugs
- Sedatives and analgesics
- Deliriogenic medications
- Neurological
- Seizures
- NCSE
- Seizures
- Metabolic causes
- Electrolyte abnormalities
- Hepatic encephalopathy
- Uraemic encephalopathy
- Acidosis
Particularly metabolic.
- Drugs
- Complete any outstanding investigations
- Neurological exam at 72 hours
Good outcome is more likely with any of:
- M4/5
- MRI with at worst isolated DWI lesion
- EEG continuous background <12 hours from ROSC
- EEG reactive background <24 hours from ROSC
- N20 SSEP >4μV >48 hours from ROSC
Poor outcome is very likely with clinical picture of severe widespread brain injury and:
- Bilateral unreactive pupils >72 hours from ROSC
- Bilateral absent N20 SEEP >48 hours from ROSC
Poor outcome is likely with clinical picture of severe widespread brain injury and:
- CT with diffuse loss of grey-white differentiation and sulcal effacement >48 hours from ROSC
- MRI-DWI with diffuse restricted diffusion at 2-7 days post ROSC
- EEG with background or burst suppression >72 hours from ROSC
Indeterminate
Continue support and observation if:
- There are no reliable predictors of poor outcome
- More time needed to ascertain patients wishes
Key Studies
Hypothermia:
- Patients with cardiac arrest due to hypothermia have good outcomes despite prolonged resuscitation
- Hypothermia has several potentially beneficial effects:
- Anticonvulsant
- Anti-inflammatory
- ↓ Cerebral oedema and ICP
- ↓ CMRO2 and ↓ HIE
- Hypothermia also has several potential harms
- ↓ HR and ↓ CO
- Arrhythmias
- ↑ QTc
- ↓ Immune function
- ↓ Rate of drug metabolism
- Hyperglycaemia
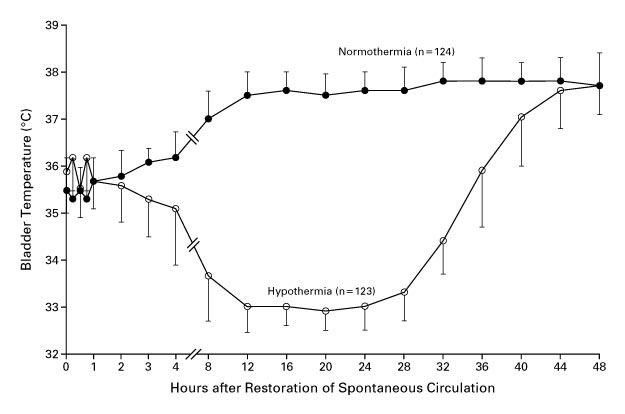
- HACA (2002)
- 275 non-pregnant European adults with witnessed shockable cardiac arrest of presumed cardiac origin
- Multicentre, assessor-blinded, block-randomised RCT
- Favourable outcome defined as CPC of 1-2; no clear power calculation
- Hypothermia vs. standard care
- Hypothermia group
- 32-34°C with surface cooling for 24 hours
- Passive re-warming after 24 hours
- Standard care group
- Hypothermia group
- Significant ↑ in favourable neurological outcome (55% vs. 39%) and ↓ in mortality (41% vs. 55%) in hypothermic group
- Normothermia group became hyperthermic after ~ 12 hours
- Stopped early for slow recruitment
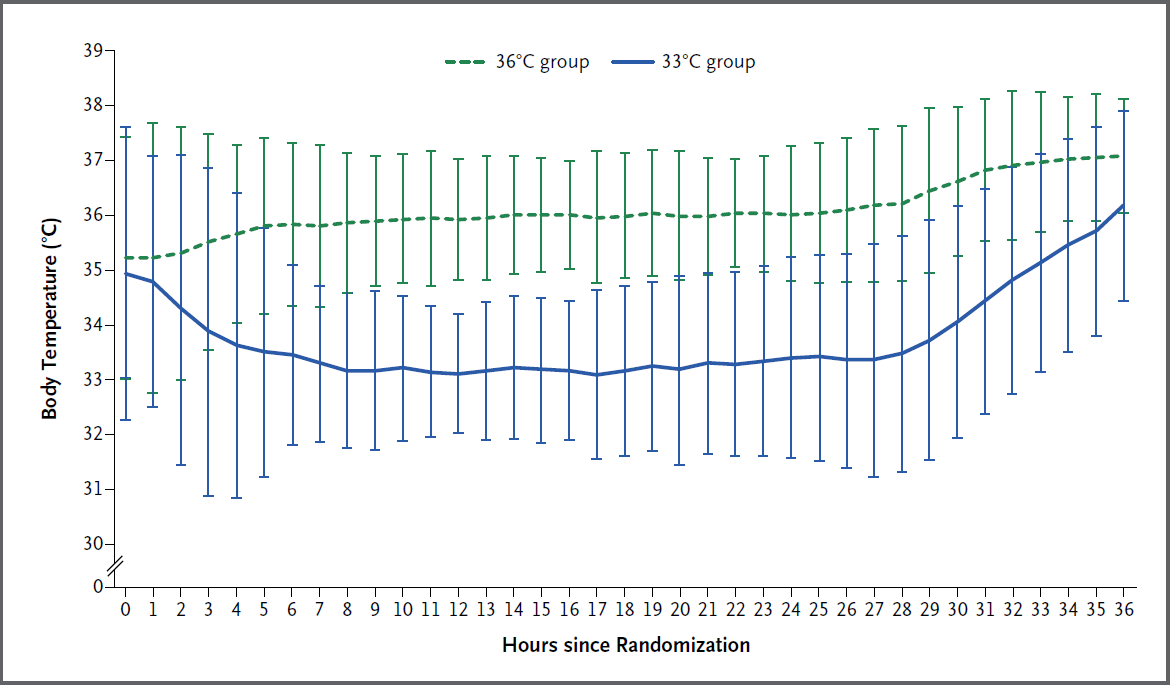
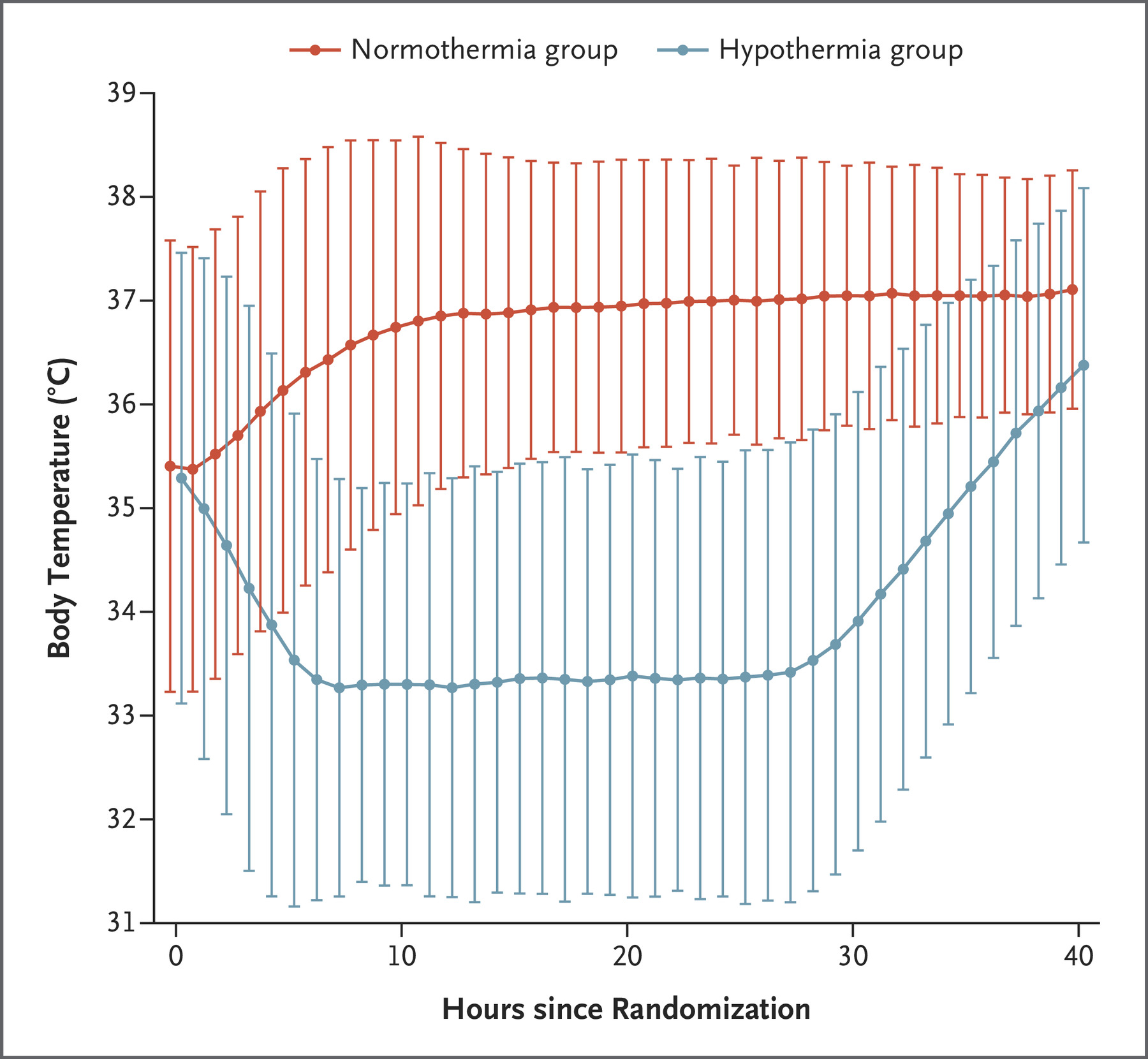
- TTM (2013)
- 950 adults with OOHCA from presumed cardiac cause and GCS <8
- Multicentre (36), assessor blinded RCT
- 900 patients provide 90% power to detect 20% ↓ in hazard ratio for death
This is ~11% ARR, which is very ambitious. - Therapeutic hypothermia at 36°C vs. 33°C
Both groups:- Targeted management for 28 hours
- Invasive or surface cooling
- Gradual warming to 37°C by 0.5°C/hr
- Avoidance of fever for 72 hours
- No mortality difference (50% vs. 48%; hazard ratio 0.89 (CI 0.89 to 1.28))
But probably underpowered for this outcome. - Reasonably good separation between groups
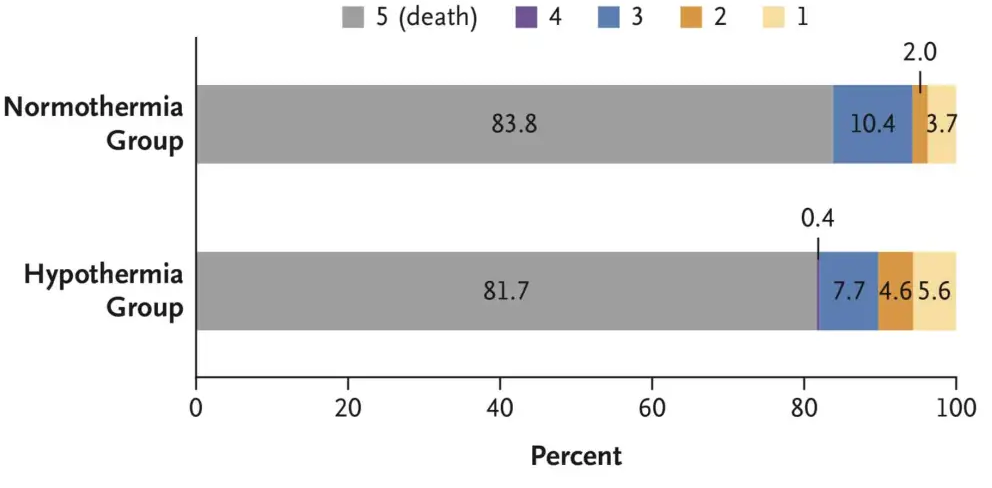
- HYPERION (2019)
- 584 non-pregnant, non-lactating Frenchpersons without end-stage liver disease post IHCA or OOHCA with a non-shockable rhythm of any cause with GCS <8 prior to admission, with <10 minute no-flow time and <60 minute low-flow time, not on obscene doses of vasopressors (<1ug/kg/min of nor/adrenaline)
- Randomised, single assessor, assessor-blinded, multi-centre RCT
- 80% power for 9% ↑ in survival with favourable neurological outcome, assuming 14% in control group
- Hypothermia (33°C) vs normothermia (36.5-37.5°C)
- Hypothermia
- Maintained for 24 hours
- External or internal active devices used
- Rewarmed at 0.25-0.5°C/hr
- Sedation to RASS -5
- Normothermia
- Maintained for 48 hours
- External or internal active devices used
- Sedation to RASS 0
- Routine sedation only for first 12 hours
- Hypothermia
- ↑ Survival with favourable outcome in hypothermia group (10.2% vs. 5.7%)
Fragile result, particularly with subjective outcome. - 30% had no bystander CPR
- 4-9% were unwitnessed arrests (lower in hypothermia group)
- 5% of control group had fevers
- Greater overlap of temperatures compared to TTM
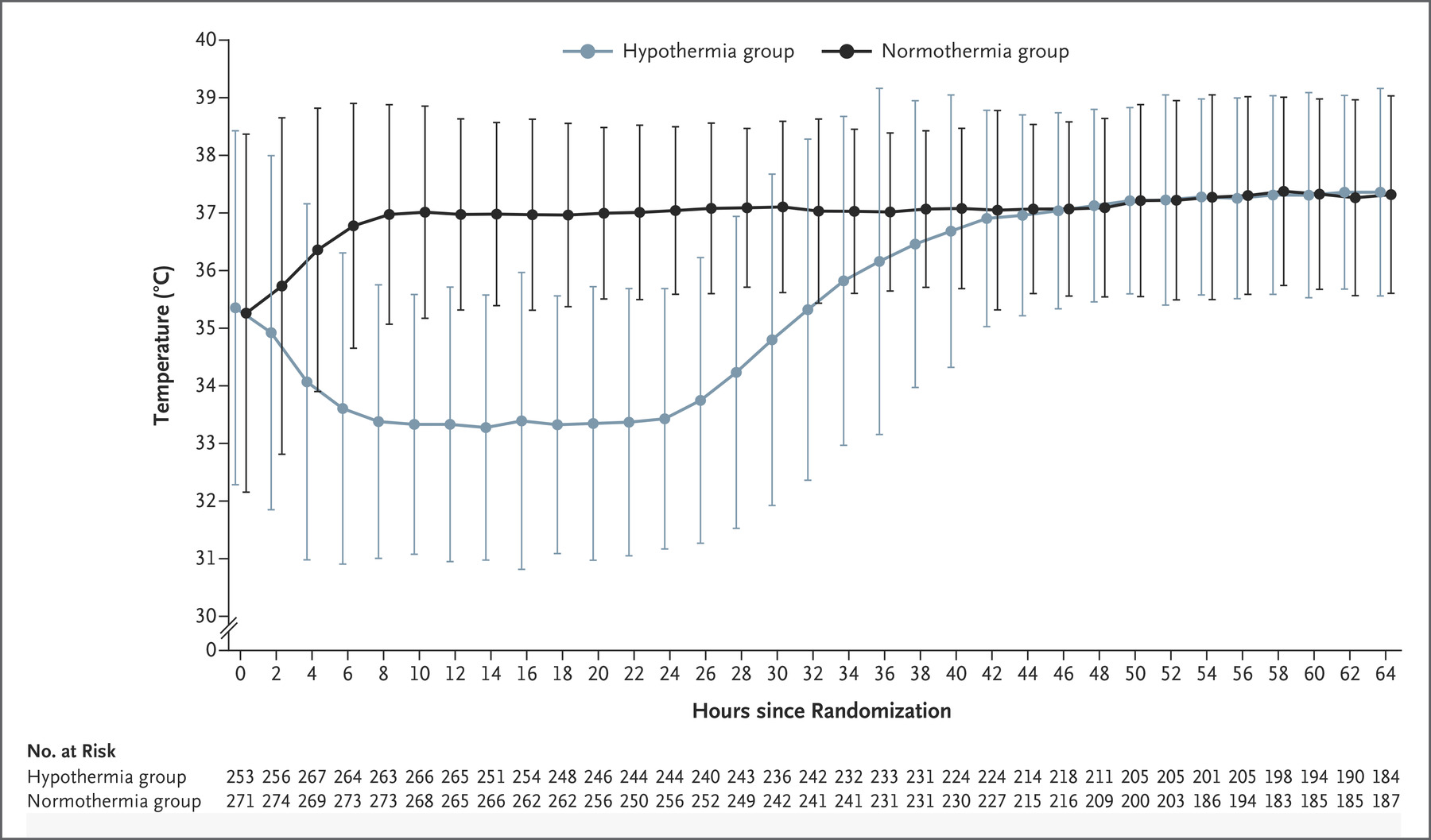
- TTM2 (2021)
- 1861 non-pregnant patients across 14 countries with witnessed OOHCA with sustained ROSC and FOUR score <4 without: ECMO, treatment limitations, ICH
- International, multi-centre, parallel group RCT
- Randomised to hypothermia (33°C) vs. normothermia (36°C)
- Hypothermia group
- Rapidly cooled with cold IVT and active internal or external cooling
- Rewarming commenced after 28 hours at <0.3°C/hr
- Normothermia group
- Cooled to ⩽37.5°C
- Less-invasive therapies initiated first
- Both groups had temperature managed using a feedback-controlled system
- Hypothermia group
- Median temperature in hypothermia group at 3 hours was 34°C, reflecting degree of difficulty achieving hypothermia
- No difference in 180 day mortality (50% vs 48%)
- ↑ Arrhythmias in hypothermia group (24% vs. 16%)
- Definitive trial on this question
References
- Sandroni C, D’Arrigo S, Nolan JP. Prognostication after cardiac arrest. Critical Care. 2018;22(1):150. doi:10.1186/s13054-018-2060-7