Rhabdomyolysis
Clinical syndrome characterised by widespread destruction of skeletal muscle leading to massive release of intracellular contents into the bloodstream, leading to:
Crush syndrome is a related entity which occurs when a crush injury leads to rhabdomyolysis but also prevents venous return from the affected limb, limiting systemic sequelae.
Relief of the crushing force (generally during extraction) results in reperfusion and ischaemic washout, which may precipitate profound haemodynamic instability or hyperkalaemic arrest.
- HAGMA
- ↑ K+
- ↑ PO4
Causing a subsequently ↓ Ca2+. - Hyperuricaemia
- ↑ Mg2+
Suggests significant concomitant AKI, due to ability of a functioning kidney to rapidly normalise magnesium levels.
Epidemiology and Risk Factors
At-risk groups include:
- Males
- Morbidly obese
- Statin users
- Post-operative
Pathophysiology
Common pathway of muscle destruction:
- Loss of cellular ATP ↓ efficacy of membrane pumps, resulting in intracellular Na+
- Secondary ↑ in Ca2+ occurs as 2Na+/Ca2+ pumps activate to correct ↑ Na+
- ↑ Intracellular Ca2+ activates various proteases, which destroy cellular and mitochondrial membranes
- Muscle cells necrose, releasing cytotoxic intracellular machinery
- Myoglobin may precipitate, causing renal tubular obstruction
This occurs due to interaction with the Tamm-Horsfall protein, and is accelerated in acidic conditions. - Hydroxyl radicals lead to lipid peroxidation and tubular sloughing
- Metabolic acidosis promotes myoglobin cast formation in the DCT
- Myoglobin may precipitate, causing renal tubular obstruction
Aetiology
- Neuromuscular
- Seizures
- Fluid and electrolyte
- DKA
- Hypokalaemia
- Hypophosphataemia
- Hypocalcaemia
- Traumatic
- Crush injury
- Compartment syndromes
- Burns
- Prolonged lie
- Infective
- NSTI
- Influenza
- EBV
- Primary HIV
- Legionella
- Environmental
- Heat injury
- Exercise
- Toxic
- Statins
- MH
- Serotonin syndrome
- Propofol infusion syndrome
- Alcohol
- Delirium tremens
- Congenital
- Various mitochondrial disorders
- Lipid metabolic disorders
- Idiopathic
Clinical Features
- Muscle pain
- Weakness
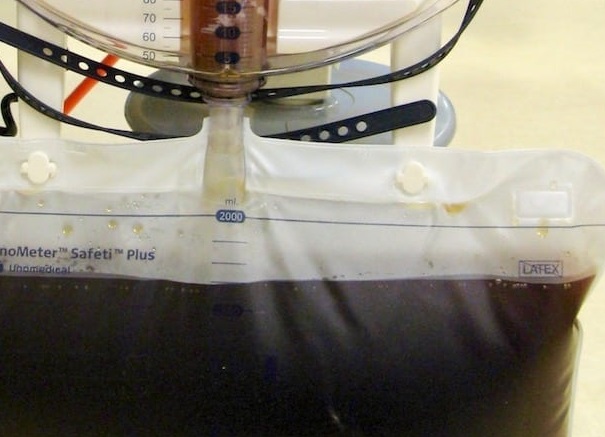
- Dark-tea coloured urine
Requires 100mg/dL of myoglobin, therefore not all cases of rhabdomyolysis develop frank myoglobinuria. - Oligo-anuria
- Intravascular volume depletion
Due to tissue oedema.
Assessment
History
Exam
Investigations
Bedside:
Laboratory:
- Blood
- ↑ K+
- ↑ PO4
- ↓ Ca2+
- ↑ AST
- ↑ LDh
- CK
Generally 5-10× ULN (~1000-2000) U/L is diagnostic, through values can rise much higher.- Rise during first 12 hours
- Peak at 3-5 days
- Return to baseline over following 6-10 days
- Myoglobin
Pathognomonic, but rarely measured. - ↓ Urea:Creatinine ratio
Due to ↑↑ creatinine, secondary to muscular destruction.
- Urine
- Myoglobin
- Dipstick
Also interactions with myoglobin - myoglobinuria can be inferred with a positive (for blood) dipstick with no red cells in the sediment.
Imaging:
Other:
Diagnostic Approach and DDx
Management
- Early, aggressive volume resuscitation
- Limit degree of AKI
- Target urine output >300ml/hr
- Consider RRT
- Avoid correcting calcium
Resuscitation:
- C
- Volume resuscitation
Often in the order of litres per day, targeting a urine output of >300mL/hr in adults.
- Volume resuscitation
- F
- Correct electrolytes
- Rapid correction of hyperkalaemia
- Avoid correction of calcium to ↓ risk of calcium-phosphate precipitation
- Correct electrolytes
Specific therapy:
Urinary alkalinisation is covered under Urinary Alkalinisation.
- Pharmacological
- Mannitol
Consider if volume resuscitation does not lead to adequate UO. Avoid in anuric patients. - Sodium Bicarbonate
Reasonable to correct systemic acidosis. Urinary alkalinisation:- Is sometimes recommended
- May ↓ myoglobin toxicity by limiting myoglobin cast formation
- Can be abandoned if urinary pH does not ↑ to >6.5
- Mannitol
- Procedural
- RRT
Effectively clears myoglobin.
- RRT
- Physical
Supportive care:
- F
- Avoid replacing calcium
Disposition:
Preventative:
Marginal and Ineffective Therapies
- Loop diuretics
Can be considered if inadequate urine output is not achieved with volume resuscitation and mannitol.
Anaesthetic Considerations
Complications
- Death
20-60% among ICU patients with rhabdomyolysis. - F
- AKI
10-60% of cases. - ↑ Ca2+
May complicate renal recovery, which occurs due to mobilisation of precipitated calcium and normalisation of PO4.
- AKI
- I
- Soft tissue CaPO4 deposition
Prognosis
Key Studies
References
- Chavez LO, Leon M, Einav S, Varon J. Beyond muscle destruction: a systematic review of rhabdomyolysis for clinical practice. Critical Care. 2016;20(1):135. doi:10.1186/s13054-016-1314-5
- Bosch X, Poch E, Grau JM. Rhabdomyolysis and Acute Kidney Injury. New England Journal of Medicine. 2009;361(1):62-72. doi:10.1056/NEJMra0801327