Neurological Examination
The neurological exam comes in an escalating level of detail, depending on the level of consciousness of the patient:
Testing and diagnosis of brain death is covered under Brain Death.
- Paralysed
- Pupils
- Unconscious
- Pupils
- Eye position
- Respiratory pattern
- Limited cranial nerves
- Limited peripheral motor
- Reflexes
- Uncooperative
- Variable
- Cooperative
- Cerebellar exam
- Detailed cranial nerves
- Detailed peripheral motor
- Detailed peripheral sensory
Assessing Level of Consciousness
- A rigorous approach improves reproducibility and reliability
- GCS score is the sum of the best result in any limb
In a patient with an unclear level of consciousness:
Vertical eye movements (but not always lateral) are preserved in locked-in syndrome.
Avoid asking the patient to squeeze hands - this may be a grasp reflex.
Report the GCS in its constituent components, e.g. E2VTM3.
- Ask to blink and to look up/down
This assesses for locked-in syndrome. - Ask for an unambiguous action (e.g. thumbs up, wiggle toes) to assess hands and feet
- If no response, perform a painful stimulus to determine the GCS
- Centrally first
Supraorbital pressure, jaw thrust. Allows assessment for localisation. - Peripherally if no central response
- Centrally first
| Score | Eye | Verbal | Motor |
|---|---|---|---|
| 6 | - | - | Obeys unambiguous command. |
| 5 | - | Orientated. Coherent and appropriate response. | Moves towards pain in a meaningful attempt to alleviate it. |
| 4 | Open spontaneously. | Confused. Appropriate (but incorrect) response. | Withdraws to pain. |
| 3 | Opens to voice. | Inappropriate response. Response does not match questions. | Abnormal flexion (decorticate posturing) to pain. |
| 2 | Opens to pain. | Incomprehensible response. Moaning/sounds, but no words. | Abnormal extension (decerebrate posturing) to pain. |
| 1 | No response. | No response. | No response. |
Levels of Consciousness
| Level | Definition |
|---|---|
| Clouded | Mild impairment:
|
| Confusion/delirium | Moderate impairment:
|
| Lethargy Somnolence Obtundation |
Impaired state from which a patient can be transiently roused from a mild to moderate stimulus |
| Stupor | Impaired state from which a patient can be very briefly roused by a repeated, vigorous stimuli |
| Coma | Impaired state from which a patient cannot be aroused |
Interpretation of Motor Response
Response to a central stimulus suggests the location of a possible lesion
| Response | Location |
|---|---|
| Localisation |
|
| Withdrawal |
|
| Upper limb flexion |
|
| Upper limb extension |
|
| Lower limb triple flexion |
|
| Decorticate posturing |
|
| Decerebrate posturing |
|
| Absent |
|
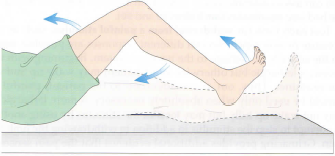

Decorticate posturing describes flexion and adduction of the upper limbs combined with extension of the lower limbs.

Decerebrate posturing describes adduction, extension, and pronation of the arms and wrists combined with extension of the lower limbs.
Pupils
Bedside assessment:
- Size
Normal is ~2-5mm, dependent on ambient light. Pupil size suggests aetiology of the lesion:- Small
- Drugs
Opioids and clonidine. - Pontine lesions
- Drugs
- Semi-dilated and unresponsive
Midbrain lesions. - Large and unresponsive
CNIII compression.
- Small
- Asymmetry
Anisocoria defined as a size difference >1mm.- Large and unresponsive
- Ipsilateral CN III lesion
May be secondary to uncal herniation. - Adie’s Pupil
Idiopathic syndrome of mydriasis and delayed response to light; may occur in one or both pupils.
- Ipsilateral CN III lesion
- Large and unresponsive
- Reactivity
- Afferent pathway via CN II
- Efferent pathway via CN III
- Abnormalities between direct and consensual reflexes allow localisation of the lesion to a particular neural pathway
- Light reactivity is usually maintained in durg or toxin induced mydriasis
Normal pupil size changes with age:
- Children: 7mm
- Adults: 5-6mm
- Elderly: 4-5mm

Detailed assessment:
- Papilloedema
Presence suggests ↑ ICP, though this may not be present (especially acutely).
Eye Position
Gaze and non-voluntary eye movements can be used to localise a brain lesion:
- Any deviation from the mid-position is abnormal
- Any difference in horizontal or vertical axial position between each eye is abnormal
| Eye Position | Lesions |
|---|---|
| Tonic conjugate upward gaze |
|
| Intermittent conjugate upward gaze |
|
| Horizontal conjugate gaze |
|
| “Ping-pong gaze” |
|
| Tonic conjugate downward gaze |
|
| Ocular dipping |
|
| Convergent nystagmus |
|
| Ocular bobbing |
|
| Skew deviation |
|
Horizontal conjugate gaze occurs towards an anatomical lesion and away from an epileptic focus.
A ping-pong gaze describes roving eye movements that alternate from one side to the other.
Ocular dipping describes slow downward eye movement, followed by a pause at the extreme of downward gaze, and finishes with a quick return to midposition.
Respiratory Patterns
| Pattern | Presentation | Mechanism | Causes |
|---|---|---|---|
| Apneustic breathing | Deep inspiration with a pause at end-inspiration, followed by brief expiration. | ||
| Central Neurogenic Hyperventilation | Primary respiratory alkalosis (hyperventilation) |
|
|
| Cheyne-Stokes | Sinusoidal pattern of:
|
Delayed feedback between CO2 detector and effector responses. |
|
Assessing respiratory pattern in the intubated patient requires desedation and a pressure-support mode.
Cranial Nerve Examination
Unconscious Patient
- Ocular deviation
- Dysconjugate gaze is present in most patients with altered conscious state, such as anaesthesia
- Tonic deviation may be present with an ipsilateral frontal lobe lesion or a contralateral pontine lesion
Supranuclear (e.g. frontal) lobe lesions can be overcome by a oculocephalic or oculovestibular reflex, pontine lesions cannot. - Vertical (skew) deviation suggests a pontine or vestibulocerebellar lesion.
- Corneal reflex
Tests V1, III (eye movement) and VII (blink).- Wisp of cotton of gauze should be applied to the cornea
- Not the sclera or conjunctiva
- Saline (more gentle) can be used as but administration should be precise enough to strike the cornea
- Patient should not see the or hear the stimulus, otherwise this will not isolate V1.
- Not the sclera or conjunctiva
- Reflex is present if they blink or look upwards
- Wisp of cotton of gauze should be applied to the cornea

- Occulo-cephalic reflex
A milder version of the cold caloric reflex that can be performed in unconscious patients. Tests CN III, VI, VIII.- The eyes are held open and the head is rotated side-to-side or up-and-down
- The reflex is present if the eyes move in the opposite direction of head movements This is a normal response.
- Absence of the reflex is suggestive of brainstem dysfunction in the comatose patient
This is described as “doll eyes” - the eyes remain fixed relative to the head.
- Facial Sensation
- Supra orbital notch pressure
Tests CN V, VII.
- Supra orbital notch pressure
- Gag reflex
Tests CN IX, X.- Touch the posterior pharynx on each side (use a Yankauer)
- Absence is an unreliable predictor of risk of aspiration
- A positive response is retching (gag reflex) or constriction of the pharynx (palatal reflex) with elevation of the uvula
- Cough reflex
Tests CN X.- Suctioning the trachea should cause a cough response
Ensure the cervical spine is cleared before testing the oculocephalic reflex.
- Vestibulo-ocular reflex
Also known as the cold caloric reflex. Tests CN III, VI, and VIII.- Predominantly used only in brain-death testing as it may produce nausea and vomiting in the non-comatose patient
- Process:
- Head elevated to 30°
- Eyes are held open to examine for eye movements
- ~50mL of ice cold water is syringed into the patients ear
- Observe for refectory eye movements
- Wait 5 minutes before testing the opposite side
- Interpretation:
- Deviation of both eyes towards the irrigated ear, returning to the mid-position when irrigation stops
Diffuse cortical lesion. - Deviation of ipsilateral eye to irrigated ear, with no movement of the contralateral eye
Medial longitudinal fasciculus lesion.
- Deviation of both eyes towards the irrigated ear, returning to the mid-position when irrigation stops
- No response will occur in brain death
- 5 minutes should elapse before testing the other wide
Cooperative Patient
- Vision
Tests CN II.- Visual acuity
- Read
- Count fingers
- Visual fields
- Patient focuses straight ahead
- Reports when a finger is moving in each quadrant
- Visual extinction
- Form of neglect
- Patient is presented with a different number of fingers on each side
- The patient will not report seeing the fingers on the affected side when presented to both sides, but can see them when presented to the affected side alone
- Visual acuity
- Extra-ocular movements
Tests CN III, IV, VI- Patient focuses straight ahead
- Eyes follow finger in an ‘H’ pattern
- Diplopia:
- Movement limitation
- Dysconjugate gaze:
- Horizontal
- Vertical
- Facial Sensation
- Trigeminal sensation
Tests CN V1, V2, V3.
- Trigeminal sensation
- Facial Expression
Tests CN VII.- Evaluate strength and asymmetry as the patient:
- Wrinkles brow
- Closes eyes tightly
- Puff out cheeks
- Smiles
- Evaluate strength and asymmetry as the patient:
Cheeks cannot be puffed out if a patient has a cuffed tracheostomy, as they cannot expire into their oropharynx.
- SCM and trapezius
Tests CN XI.- Evaluate strength as the patient:
- Shrugs shoulders
- Turns head to each side
- Evaluate strength as the patient:
- Tongue
Tests CN XII.- Atrophy
Occurs with LMN lesion. - Fasciculations
Occurs with LMN lesions. - Deviation
Weakness causes deviation to the affected side. - Push forcefully against inside of the cheek
- Atrophy
Peripheral Motor Exam
- Asymmetry in tone, reflexes, and plantar responses are useful to lateralise a lesion
- Symmetrical changes are rarely helpful in the unconscious patient
A lesion above the brainstem is suggested by decorticate posturing:
- Flexion of arms
- Adduction of shoulder
- Extension of legs
A lesion below or at the brainstem is suggested by decerebrate posturing:
- Extension of arms
- Internal rotation of shoulder
| Finding | UMN | LMN |
|---|---|---|
| Atrophy | No | Yes |
| Fasciculations | No | Yes |
| Reflexes | ↑ | ↓ |
| Tone | ↑ | ↓ |
| Weakness | Yes | Yes |
Observation:
- Spontaneous or localising movements
- Posturing
- Abnormal flexion (decorticate posturing)
- Abnormal extension (decerebrate posturing)
- Abnormal flexion (decorticate posturing)
- Tremors
Should be no tremors at rest in normal individuals. - Wasting
- Normal muscle bulk for age
- Symmetry of muscle bulk
- Fasciculations
- Intrinsic hand muscles
- Shoulder girdle
- Thigh
Tone:
- Passive movement of:
- Upper limb
- Shoulder
Circumduction. - Elbow
- Flexion/extension
- Pronation/supination
- Wrist
Circumduction.
- Shoulder
- Upper limb
- Joint should be able to be moved easily through its range of motion
- Divided into:
- Spasticity
Velocity-dependent, i.e. ↑ in tone is proportional to the rate of movement. Associated with UMN lesion. - Rigidity
Velocity-independent, i.e. tone is ↑ irrespective of how quickly the joint is moved. May be:- Cogwheel
Hypertonia with superimposed tremor, such that tone intermittently ↑ during movement. - “Lead-pipe”
Uniform ↑ in tone throughout.
- Cogwheel
- Flaccidity
Complete absence of tone, occurring when the muscle has no LMN innervation.
- Spasticity
Power:
- Strength of major muscle groups
- Joints should be stabilised and isolated so each is tested individually
- Assessment must consider the age, sex, fitness, and non-neurological disease state.
| Grade | Movement |
|---|---|
| 0 | Paralysis |
| 1 | Palpable or visible contraction |
| 2 | Movement with gravity eliminated |
| 3 | Antigravity movement |
| 4 | Movement against moderate resistance Additional (subjective) nuance can be documented by using 4+ or 4- for varying levels of “some” resistance. |
| 5 | Movement against full resistance |
| 5* | Expected movement against full resistance if inhibiting factors (pain, myopathy) were not contributing |
| NT | Not testable e.g. Due to immobilisation, pain, amputation, or contractures. |
Reflexes:
The deep tendon reflexes are:
- Upper limb
- Biceps
- Brachioradialis
- Triceps
- Lower limb
- Patella
- Ankle
- Look for muscle contraction rather than physical movement
- Clonus
>5 sustained involuntary contractions following stretching of a muscle. - Plantar response
Sensitive test for the presence of an UMN lesion in the corticospinal tract.- Lateral side of foot is rubbed with a blunt instrument
- Flexion of the toes is a normal (negative) response
- Extension of the hallux with fanning of the toes is a positive Babinski sign
Present as a primitive reflex in infants up to 12 months of age.
- Hoffman Reflex
Sensitive test for UMN lesion in the cervical spine.- DIP joint of the 3rd digit is stabilised and the fingertip is flicked
- Opposition of the thumb and forefinger is a positive response
Peripheral Sensory Exam
Testing of each main afferent pathway:
- Spinothalamic tracts
Pain, temperature, crude touch. - Dorsal columns
Proprioception, vibration, light touch.
Assessment process:
- Sharp and light touch
- Demonstrate to the patient what light and sharp touch will feel like
- Start distally and move proximally, crossing multiple dermatomes at each point
- Proprioception
- Have the patient close their eyes
- Grasp either side of the great toe IP joint
- Orientate the patient to what up and down will be
- Then move the toe and ask the patient to state in which direction it has been moved
- If incorrect, then move to a more proximal joint
Distal joints are typically affected first.
- If incorrect, then move to a more proximal joint
- Vibration
- Use a 128Hz tuning fork
- Place the fork over the great toe IP joint
- The patient should be able to identify when vibration occurs, and when vibration ceases
- Two-point discrimination
Useful for peripheral neuropathy.- Patient should be able to distinguish simultaneous touch from two objects >5mm apart
Cerebellar Exam
- Nystagmus
- A fast phase of nystagmus will occur towards the side of a cerebellar lesion
- Staccato speech
- Resting tremor
- Head
Known as titubation. - Upper limb
- Head
- Tests of coordination:
- Rapid alternating movements
- Finger-nose
- Finger-finger
Close eyes and outstretched arms, and attempt to place fingertips together. - Heel-shin
- Gait
- Romberg’s test
- Patient stands with eyes closed
- A positive result occurs if the patient loses balance
- Cerebellar ataxia occurs even when the eyes are open
- Sensory ataxia occurs when the eyes are closed, and is a sign of disturbed proprioception
References
- Walker MC, O’Brien MD. Neurological examination of the unconscious patient. J R Soc Med. 1999 Jul;92(7):353-5.
- Smith, Eimear, and Mark Delargy. ‘Locked-in Syndrome’. BMJ: British Medical Journal 330, no. 7488 (19 February 2005): 406–9.
- Dünser MW, Dankl D, Petros S, Mer M. Clinical Examination Skills in the Adult Critically Ill Patient. Springer International Publishing; 2018.