Airway Assessment
- Predicting an anatomically difficult airway is unreliable
- When a predicted difficult airway exists, a plan should be developed to manage that particular difficulty
- Previous difficulty with a technique is the greatest predictor of difficulty with that technique
Airway assessment involves identifying potential:
- Anatomical difficulty
- Physiological difficulty
- Situational difficulty
Anatomical Difficulty
Anatomical difficulty can be further divided into difficulty with:
- Mask Ventilation
- SAD placement
- Intubation
- FOI
- FONA
Difficulty with one technique is associated with difficulty of other techniques.
Consider elective cannulation of the cricothyroid membrane if multiple anatomical difficulties exist.
Difficult Mask Ventilation
Defined as inability to keep ventilate without:
- 2-person technique
- Airway adjuncts
- Paralysis
Assessment:
- Typically poorly predicted
May be <20% of all patients. - Risk ↑↑ with >1 risk factor
Risk Factors (MBBS MAT):
- Mallampati III/IV
- Beard
- BMI >25
- Snoring
- Male
- Age >55
- Teeth (lack of)
Teeth are numbered:- Firstly by quadrant
Top-right, top-left, bottom-left, bottom-right.- Adult teeth are quadrants 1-4 respectively
Each quadrant has 8 teeth, for a total of 32. - Deciduous (baby) teeth are quadrants 5-8
Each quadrant has 5 teeth, for a total of 20.
- Adult teeth are quadrants 1-4 respectively
- Secondly by tooth number, from medial to lateral
- Firstly by quadrant
Difficult Intubation
Risk factors (LEMON):
- Cormack and Lehane Grading:
Cook modification correlates better with time to intubate and requirement for adjuncts.
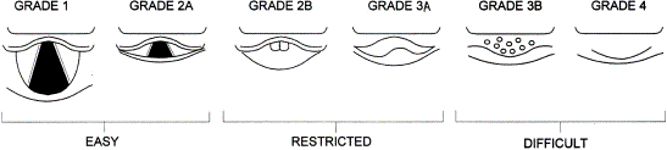
- Grades are by best view, with or without ELM or BURP
- This modification adds additional complexity
The author recommends subdividing into three tiers which have greater practical value:- Easy: Laryngeal inlet visible
- Restricted: Posterior glottic structures visible
Likely amenable to bougie. - Difficult: Epiglottis cannot be lifted/No structures visible
Likely require specialist or blind techniques, and is associated with a significantly longer intubation time.
- External anatomy
The 3-3-2 rule is a crude predictor of difficult airway:- Interincisor distance <3cm
- Thyromental distance <3cm
- Hyoid-thyroid notch distance <1cm
- Mallampati score
MP 4 is associated with >10% change of difficult intubation. - Obstruction
- Neck mobility
Ability to assume the ear-to-sternal notch position.
Difficult SAD Placement
Defined as inability to ventilate, requiring removal and tracheal intubation. SAD failure occurs in ~1% of instances, and is usually due to:
- Leak
- Obstruction
Risk Factors (PROMPT):
- Poor respiratory compliance
- Restricted mouth opening
- Obesity
- Male
- Position
Non-level operating table. - Teeth (poor)
Difficult FOI
Risks:
- FOI failure occurs in ~1.5% of instances.
- Epistaxis occurs in ~10%
- Severe epistaxis occurs in ~1.3%
Difficult FONA
Risk factors (SHORT):
- Surgery
- Haematoma
- Obesity
- Radiation
- Tumour
Physiological Difficulty
Key physiological states that affect induction are the VAPOURS:
- Ventilation
PPV may have many detrimental effects:- Reduce VR and therefore BP
- Volutrauma and barotrauma
- Gastric insufflation
- Acidaemia
Very high minute ventilation may be compensating for metabolic acidosis
- Rendering the patient apnoeic may lead to a rapid ↑ in PaCO2, fall in pH, and precipitate cardiac arrest
- Consider gentle BMV during the apnoeic period to reduce this risk
This needs to be balanced against the risk of gastric insufflation and aspiration.
- Consider gentle BMV during the apnoeic period to reduce this risk
- Use ETCO2 during preoxygenation to identify what the patients (compensating) ETCO2 is prior to induction
- Aim for an ETCO2 at least as low post-induction
- Rendering the patient apnoeic may lead to a rapid ↑ in PaCO2, fall in pH, and precipitate cardiac arrest
- Pressures
Important pressures to consider (ABG):- Airway pressures
Avoid excessive airway pressures (Aim Pplat <30 cmH2O):- Auto-PEEP
↑ RV afterload, reducing VR and subsequently BP.- Beware hypoxia secondary to impaired circulation due to this reason, and avoid ↑ minute ventilation further
Ensure adequate time for expiration, especially in patients with obstructive lung disease.
- Beware hypoxia secondary to impaired circulation due to this reason, and avoid ↑ minute ventilation further
- Barotrauma
- Auto-PEEP
- Systemic arterial pressure
Aim for a higher systemic BP prior to induction. - Pulmonary arterial pressure
PAP will also be affected by pH and PAO2. Defend the systemic MAP to maintain RV perfusion. - Gastric pressure
- Airway pressures
- Oxygenation
Hypoxia is:- What kills patients during prolonged attempts at intubation
- More important than ventilation, except at extremes of pH
A starting pH of 7.1 will lead to a pH of ~6.9 after 4 minutes of apnoea (assuming a normal VCO2). - Reduced by:
- Adequate denitrogenation
↑ FRC oxygen concentration and therefore oxygen reserve. - Lung recruitment
↑ FRC volume.
- Adequate denitrogenation
- Underlying disease
- Regurgitation
Consider the risks of aspiration and other airway contaminants (e.g. blood). - Shock Index
\(SI = {HR \over BP}\). If the SI is >1, then consider initiating vasopressors/volume prior to intubation. If using vasopressor infusions, then prepare these prior.- Dose ↓ sedatives
Up to 90%. - Dose ↑ relaxants
- Aggressively treat hypotension
- Dose ↓ sedatives
Situational Difficulty
References
- Cook TM, MacDougall-Davis SR. Complications and failure of airway management. BJA: British Journal of Anaesthesia, Volume 109, Issue suppl_1, 1 December 2012, Pages i68–i85.
- Cook TM. A new practical classification of laryngeal view. Anaesthesia. 2000. 55: 274-279.
- Nickson, C. Making it happen: Not if, when. Critically Ill Airway Course Notes. 2018.
- Levitan, R. The VAPORS and the Resuscitation Sequence of Intubation. Mayo Clinic EM. 2015.
- Steven L. Shafer. Shock Values. Anesthesiology 2004;101(3):567-568.