Tetanus
Non-communicable infection of devitalised tissue by Clostridium tetani, which produces an exotoxin that causes life-threatening:
- Muscle rigidity
Including laryngeal and respiratory muscle spasm. - Autonomic instability
Haemodynamic lability, including cardiac arrest. - Convulsions
Epidemiology and Risk Factors
Significant public health problem of the developing world, due to a combination of:
- High incidence
Major risk factors include:- Unvaccinated
- LMIC
- Elderly
- Rural
- Poor
- Unvaccinated
- Requirement for prolonged ICU care
Pathophysiology
C. tetani is a Gram positive rod and obligate anaerobe that:
- Exists in spore form in the environment
- Is non-invasive
Requires innoculation into a wound to produce infection - cannot grow in vitalised tissue. - Produces two exotoxins:
- Tetanospasmin
- LD50 0.01mg
- Haematological spread
- Uptake into motor nerve endings, and transport into nervous system
- Diffuses into interstitium with, and acts on pre-synaptic terminals of nearby neurones
Produces dysfunction of predominantly inhibitory interneurons:- Muscle spasms
- Autonomic dysfunction
Requires toxin to diffuse to lateral horns.- ↑ Sympathetic tone
- Cognitive dysfunction
- Tetanolysin
Localised tissue destruction; clinically relatively unimportant.
- Tetanospasmin
Fun Fact:
~240g of tetanospasmin could kill the entire world population.
Aetiology
Mechanisms of C. tetani innoculation include:
- Trauma
- Puncture
- Laceration
- Dog bites
- Piercings
- Skin breakdown
- Burns
- Chronic ulcers
- Dental infections
- Other devitalised tissue
- Abortion
- Childbirth
- Tetanus neonatorum
Infection of umbilical stump.
Clinical Manifestations
Presentation:
- Occurs following an incubation period
A shorter incubation period indicates ↑ severity.- Usually >2 days
- 90% <14 days
- Up to 60 days
- Usually >2 days
- Pain
- Musculoskeletal symptoms
Progression:- Stiffness
- Rigidity
- Trismus
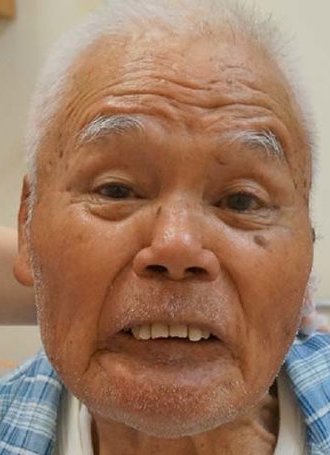
Presentation typically at this point, which occurs due to masseter spasm. - Risus sardonicus
Clenched-teeth expression relating to facial muscle spasm.
- Autonomic dysfunction
- Confined to severe cases
- Begins after muscle spasms
- Generally short-duration episodes of:
- ↑↑ Sympathetic tone
- ↑↑ Parasympathetic tone
- Including sudden cardiac arrest
Particularly in IVDU.
- Including sudden cardiac arrest
Tetanus neonatorum presents:
- ~7th day of life
- Short history of failure to feed
Diagnostic Approach and DDx
Include:
- Local disease
- Dental
- TMJ disease
- Infection
- Neurological disease
- Epilepsy
- Toxidromes
- TCA overdose
- Strychnine poisoning
Investigations
No specific laboratory findings - diagnosis is clinical.
Bedside:
- ABG
Respiratory failure.
Laboratory:
- Bloods
- UEC
Rhabdomyolysis. - CMP
- UEC
- Wound culture
May grow C. tetani.
Imaging:
Other:
Management
- Immunoglobulin to neutralise circulating toxin
- Source control/wound care
- Autonomic support
Resuscitation:
- A
- Intubation
For control of muscle spasm.
- Intubation
- B
- Mechanical ventilation
- If respiratory muscle involvement
- Muscle relaxation if spasms prevent ventilation
No particular agent is preferred.
- Mechanical ventilation
- C
- Haemodynamic control
Consider:- ↓ Catecholamine production
- Sedation
May require hefty doses, Oh’s quotes 3.4 grams of diazepam daily. - Opioids
Heavy doses may also be required.
- Sedation
- α/β Antagonists
- Clonidine
- Phentolamine, phenoxybenzamine
- Esmolol
- MgSO4
Target 2.4-4mmol/L. May also assist in ↓ spasm.
- ↓ Catecholamine production
- Haemodynamic control
Specific therapy:
- Pharmacological
- Human antitetanus immunoglobulin
- 500 IU
- Should be given to all patients who are not known to be immunised on presentation
- Binds circulating toxin
- Antibiotics
Spores and bacteria are destroyed by:- Metronidazole 500mg IV Q6-8H for 10 days
Preferred. - Penicillin G 1-3MU IV Q6H for 10 days
- Metronidazole 500mg IV Q6-8H for 10 days
- Human antitetanus immunoglobulin
- Procedural
- Wound care
Washout of contaminated wounds. - Source control
- Wound care
- Physical
Supportive Care:
- C
- Haemodynamic control
- Labetalol
- Magnesium
- Clonidine
- Haemodynamic control
Disposition:
- ICU
Preventative:
- Tetanus toxoid vaccine
- Cheap
- Three doses for full course
2nd at 6-12 weeks, 3rd at 6-12 months. - Booster every 10 years
- Occasionally results in local tetanus
Spasm of limb or muscle. - Frequent doses may result in non-life threatening immune symptoms
Neonates have immunity via maternal antibodies until 3 months, and vaccination of pregnant women will protect children produced within 5 years.
Marginal and Ineffective Therapies
Complications
- Death
- B
- Respiratory failure
- C
- Cardiac failure
↑ Catecholamines. - Hypertensive crises
- Cardiac failure
- D
- Spasm
- F
- Rhabdomyolysis
Prognosis
- Death
- 80% without ICU care
- 10% with mechanical ventilation
- More common with:
- Systemic tetanus
- Cephalic tetanus
Secondary to head and neck injuries with CN involvement. - Age
- C
- Arrhythmias
- Cardiac failure
- D
- Spasm
- Most resolve within 1-3 weeks
- Residual stiffness may remain
- Cognitive changes
- Spasm
Key Studies
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.