Acute Liver Failure
Rapidly progressive, life-threatening development of coagulopathy (INR >1.5), encephalopathy, and jaundice in a patient with a previously normal liver secondary to massive liver parenchymal injury.
Acute Liver Failure is distinct from:
- Acute Liver Injury
Coagulopathy and jaundice in absence of encephalopathy. - Acute on Chronic Liver Failure
Acute decline in liver function in patients with chronic liver disease.
ALF is subclassified by time interval between jaundice and encephalopathy into:
- Hyperacute
Encephalopathy within 7 days. Typically:- Severe encephalopathy, coagulopathy, ↑ ICP, and very deranged LFTs
Encephalopathy usually preceeds jaundice. - Common aetiologies: paracetamol, viral hepatitis
- Higher rate of spontaneous recovery
- Severe encephalopathy, coagulopathy, ↑ ICP, and very deranged LFTs
- Acute
Encephalopathy within 28 days. Typically:- More gradual decline
- Common aetiologies: idiosyncratic drug reactions, viral hepatitis
- Subacute
Encephalopathy within 3 months. Typically:- Less deranged LFTs
- Common aetiologies are drug or immune-mediated disease and unlikely to be pregnancy-related or viral.
- Poorest recovery in absence of transplantation
- Greatest degree of jaundice
Hepatic encephalopathy may complicate either acute liver failure or chronic liver disease, and is covered under Hepatic Encephalopathy.
Epidemiology and Risk Factors
Rare:
- 400 cases annually in the UK
Pathophysiology
Pathological processes:
- Direct hepatocyte damage
- Immune response
- Local
- Systemic
- MODS
- Cerebral dysfunction
- Oedema
- Altered autoregulation
Aetiology
- Vascular
- Ischaemia
- Budd-Chiari Syndrome
Hepatic vein thrombosis, usually with an underlying procoagulant condition.
- Infection
- Hepatitis A
Infection rarely leads to liver failure (<1%) and contributes to ~10% of infective cases. - Hepatitis B
25-75% of viral cases. Reactivation may occur in immunosuppressed patients. - Hepatitis C
Common cause of CLD but rarely causes acute failure. - Other viruses may cause rarely infection in the immunocompromised:
- EBV
- Measles
- HSV 1/2
- Dengue
- Yellow fever
- Lassa
- Hepatitis A
- Autoimmune
- Drugs/toxins
- Paracetamol
50-70% of cases in the developed world. Occurs due to:- Depletion of hepatic glutathione
Consumed in conjugating NAPQI, a Phase I metabolite of paracetamol. - NAPQI accumulation causes direct hepatocyte injury
- Depletion of hepatic glutathione
- Aspirin
Reye’s syndrome. - Herbal
- Halothane
- Antituberculosis drugs
- Alcohol
- Ecstasy
- Amanita phalloides
Mushroom poisoning. Usually presents with diarrhoea, followed by hepatic necrosis at 48-72 hours.
- Paracetamol
- Pregnancy-related
- Acute fatty liver of pregnancy
- Severe pre-eclampsia
- Liver rupture
- Hyperthermia
- Other
- Wilson disease
- Haemophagocytic syndrome
Causes vary substantially with geography.
Clinical Features
History
- Overdose
- CNS
- Encephalopathy
- Confusion
- Agitation
- Encephalopathy
- GI
- Nausea/Vomiting
- Diarrhoea
Examination
- Asterixis
- Intracranial hypertension
- Hyperreflexia
- Clonus
- Hypertonicity
- Cushing’s triad
- Jaundice
Diagnostic Approach and DDx
Investigations
Laboratory:
- Blood
- Liver function testing
Severity and pattern of injury:- Hepatocellular
- Cholestatic
- Point of care coagulation studies
May be more accurate than standard assays. - Coagulation studies
- Synthetic function
- Lactate
Failure of hepatic clearance. - Ammonia
Neurotoxin responsible for much of hepatic encephalopathy.- >100μmol/L predicts the onset of encephalopathy
- >150-200μmol/L predicts risk of herniation
- ↑ Ammonia may reflect:
- Hepatic metabolic dysfunction
Degree of hepatic dysfunction typically correlates with ammonia level, though not with the degree of encephalopathy. - ↑↑ Protein intake
- ↑ GI ammonia production
Produced by gut bacteria. - ↓ Clearance
Urea cycle disorder.
- Hepatic metabolic dysfunction
- UEC
- AKI
- Electrolyte derangements
- FBE
- Anaemia
- Thrombocytopaenia
- Concurrent infection
- Lipase/amylase
- Associated pancreatitis
- Paracetamol level
- LDH
Malignancy. - Viral screen
Aetiology. Include:- Hepatitis A
- Hepatitis B
Core antigen indicates infection. Surface antigen often negative. - Hepatitis C
Positive antibodies indicate infection. - Hepatitis E
Positive antibodies indicate infection. Usually faecal-oral, though a subtype is transmissable by blood. - EBV
- HSV
- VZV
- HIV 1/2
- Autoimmune screen
- ANA
Autoimmune. - Anti-smooth muscle Ab
Autoimmune. - Anti-mitochondrial Ab
Primary sclerosing cholangitis. - Copper studies
Wilson’s disease.
- ANA
- Blood cultures
- Pregnancy test
- Liver function testing
- Urine
- Drug screen
- Paracetamol
- Drug screen
Albumin is relatively unhelpful in ALF. LFTs are useful for determining cause.
INR is more useful than bilirubin as it has a shorter half-life and so is more useful for tracking trends.
Imaging:
- TTE
- RV function
- Transplant assessment
- Liver ultrasound
- Splenomegaly
- Ascites
- Nodularity
- Hepatomegaly
- Portal blood flow
- Portal patency
- CT
Triple-phase liver.
Other:
- Liver biopsy
- Rare in acute setting due to coagulopathy
Transjugular route safest. - Non-specific necrosis most common finding
- May be useful in diagnosis of:
- Autoimmune
- Wilson’s disease
- Rare in acute setting due to coagulopathy
Management
- Prevent cerebral oedema and treat concurrent Hepatic Encephalopathy
- Manage vasodilatory shock
- Treat concurrent sepsis
Gram negative and fungal. - Manage coagulopathy
- Early identification of patients for transplant
- Significant improvement in outcomes with emergency liver transplantation
- Early escalation to critical care and early referral to a specialist centre is essential
Resuscitation:
Specific therapy:
- Paracetamol overdose
- N-acetylcysteine (NAC)
- Cornerstone of therapy as early administration results in significant reduction in mortality (to <1%), though even late administration may improve outcome
- Dosing based on Prescott nomogram
- N-acetylcysteine (NAC)
- Viral hepatitis
- Antivirals
- Hepatitis B
- Lamivudine
Benefit if given early.
- Lamivudine
- Alcoholic hepatitis
- Autoimmune hepatitis
- Steroids
- Mushroom poisoning
- Forced diuresis
↑ Renal clearance of toxin. Avoid hypovolaemia.
- Forced diuresis
- Wilson’s disease
- D-Penicillamine
Chelates copper. Withdrawal of chronic treatment may precipitate failure.
- D-Penicillamine
- Hepatic vein thrombosis
- Thrombolysis
- Clot retrieval
- TIPS
Management of paracetamol overdose is covered under Paracetamol.
Supportive care:
Invasive intracranial pressure monitoring associated with ~10% intracranial haemorrhage rate.
- A
Consider securing airway if:- High grade (III/IV) hepatic encephalopathy
- Need for transfer
- B
- Lung protective ventilation
ARDS risk. - Drain pleural effusions
- Lung protective ventilation
- C
- Volume resuscitation
Can be aggressive in absence of pulmonary hypertension. - MAP 65-70mmHg
Or higher if targeting CPP with concurrent hepatic encephalopathy.- Noradrenaline 1st line
- Vasopressin 2nd line
- Corticosteroids for vasopressor-refractory shock
- Hydrocortisone 50mg IV Q6H
- Volume resuscitation
- E
- ↓ BSL
Use high-concentration dextrose to avoid cerebral oedema/↓ Na+.
- ↓ BSL
- F
- RRT
- Use bicarbonate buffered solutions
Avoid citrate! - CRRT strongly preferred for haemodynamic stability
- Haemodiafiltration preferred
Dialysis is probably more effective than filtration, but both mechanisms are effective. - In addition to standard indications, initiate for:
- Hyperammonaemia (>100μmol/L)
- Aim <60μmol/L once commenced
- High doses (45-90mL/kg/hr) are often used to ↑ ammonia clearance
↑ Rate by 50% until target ammonia reached.
- Hyperthermia
- Hyperammonaemia (>100μmol/L)
- Use bicarbonate buffered solutions
- Avoid positive fluid balance
- RRT
- G
- Early low-protein enteral feeding
- May have ↑ metabolic requirements
- Feeding may need to be interrupted if ammonia ↑
- May have ↑ metabolic requirements
- Hyperammonaemia
- Lactulose
Controversial. May ↓ hepatic encephalopathy but lead to gaseous intestinal distension.
- Lactulose
- PPI
- Drain ascites
For haemodynamic benefit. - Extra-corporeal hepatic support
Broadly, ↓ encephalopathy and ↑ haemodynamic function without mortality benefit.- Should be regarded as experimental
- Can be considered for severe refractory vasodilatory shock
- Include:
- Coupled Plasma Filtration Adsorption (CPDFA)
- Molecular Adsorbant Recirculation System (MARS)
- Single Pass Albumin Dialysis (SPAD)
- Underlying mechanism is either:
- Biological
Using human/porcine cells. - Mechanical
Molecular filtration.
- Biological
- Early low-protein enteral feeding
- H
- Coagulopathy
- Patients may be prothrombotic, anti-thrombotic, or fibrinolytic
- Assays themselves (both coagulation profiles and point-of-care testing) may not correlate with the observed clinical effect
- Treat if bleeding or:
- Prior to procedures
- INR >5
May require continuous FFP infusion in unstable patients. - Fibrinogen <0.8
- Platelets <20×109/L
- Therapeutic options:
- Vitamin K 10mg IV daily
Very reasonable, probably ineffective in the majority of patients. - PCC
Useful for factor replacement without volume load. - Fibrinogen
Target >1.5g/L. Dysfibrinogenaemia is likely in chronic disease.
- Vitamin K 10mg IV daily
- Individualisation of thromboprophylaxis
- Coagulopathy
Disposition:
- Liver transplant centre
Referral if:- Hepatic encephalopathy
- Ammonia >100μmol/L
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
- Death
- Intracranial hypertension
Most common mechanism in untreated disease. - Sepsis/multiorgan failure
- Intracranial hypertension
- A
- Unprotected airway
- B
- ARDS
Relatively intolerant of permissive hypercapnoea due to ↑ ICP concerns. - Pleural effusions
- ARDS
- C
- Distributive shock
- D
- Intracranial hypertension
Usually develops rapidly with little time for adaptation. - Hepatic encephalopathy
- Intracranial hypertension
- F
- AKI (hepatorenal syndrome)
40-80% of cases.- ↑ In paracetamol toxicity (directly nephrotoxic)
- AKI (hepatorenal syndrome)
- G
- ↓ BSL
- Pancreatitis
- Ascites
- H
- Coagulopathy
Clinical manifestations often not in consistent with assays. - Bone marrow suppression
- Thrombocytopaenia
- Coagulopathy
- I
- Infection
↑ Susceptibility due to functional immunosuppression.
- Infection
Prognosis
Spontaneous recovery occurs in only 40%. Factors:
- Age
↑ Mortality with ↑ age. - Aetiology
↓ Mortality with pregnancy-related causes. - Acuity
↑ Mortality with ↑ acuity.
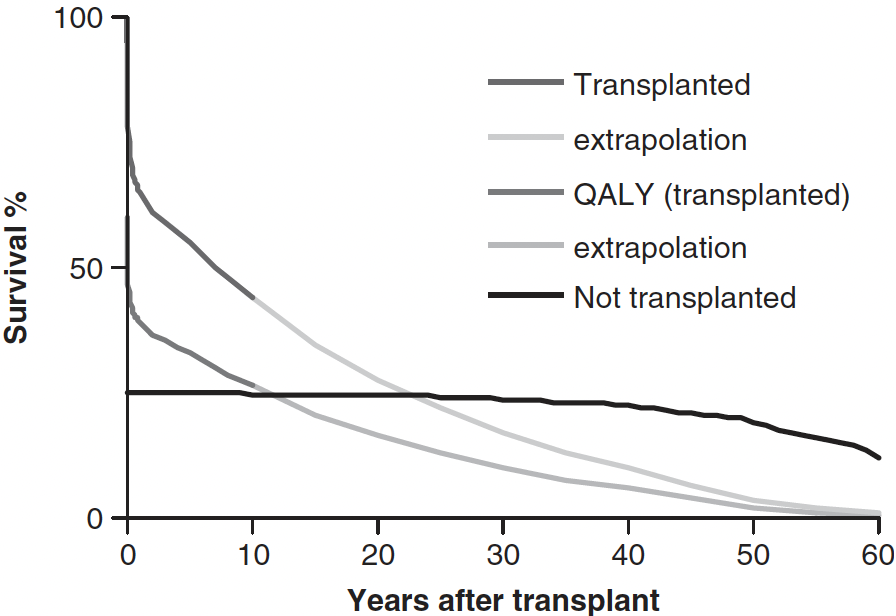
Transplantation:
- 80% 5-year survival following liver transplant for ALF
Scoring
Eligibility for transplantation is determined using one of the prognostic scores, such as MELD or the King’s College criteria.
| Paracetamol Toxicity | Other Cause |
|---|---|
|
|
Or:
|
Or 3 of:
|
The King’s criteria are the most widely used scoring system to predict liver transplant. However, there are several important caveats to use of the tool:
- Development and validation occurred at a single centre in the 1970s and 1980s
- Medical management of hepatic failure in generation and paracetamol toxicity in particular has improved significantly in the interim
- Patients at King’s who received transplantation typically had a better prognosis than those who didn’t
- Patients meeting criteria who were not listed had a 9% survival
- Patients meeting criteria who were listed but did not receive a transplant had 17% survival
- Moderate specificity
~90% specific for need of transplantation; ~15% of patients meeting criteria will survive without transplantation. - Low sensitivity
~60%; such that 40% of patients who do not meet criteria may still die from liver failure. - Patients who survive the acute liver injury and who do not receive a transplant are spared the cumulative mortality risk and quality of life impairments that come with having a liver transplant
- Patients without cerebral oedema or haemodynamic instability tend to survive with standard ICU care
Key Studies
References
- Aziz, Riaz, Jennifer Price, and Banwari Agarwal. Management of Acute Liver Failure in Intensive Care. BJA Education 21, no. 3 (March 2021): 110–16. https://doi.org/10.1016/j.bjae.2020.11.006.
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.
- Van Eldere A, Pirani T. Liver intensive care for the general intensivist. Anaesthesia. 2023;78(7):884-901.
- Warrillow SJ, Bellomo R. Preventing Cerebral Oedema in Acute Liver Failure: The Case for Quadruple-H Therapy. Anaesth Intensive Care. 2014;42(1):78-88.
- Ding GKA, Buckley NA. Evidence and consequences of spectrum bias in studies of criteria for liver transplant in paracetamol hepatotoxicity. QJM. 2008 Mar 18;101(9):723–9.