Erythrocytes
Red cell indices reported on a full blood exam may include:
Red cell indices essentially describe:
- How much haemoglobin there is
- How many cells the haemoglobin is distributed into
- Haemoglobin
Concentration of haemoglobin in blood.- Indicator of oxygen carrying capacity
- Haematocrit
Proportion of blood volume made up of erythrocytes.- Usually ~3x the haemoglobin
- Red cell count
Number of cells per microlitre. - MCV
Average volume of individual erythrocytes.- Classifies anaemia into microcytic, macrocytic, or normocytic
- MCH
Average amount of haemoglobin per erythrocyte. - MCHC
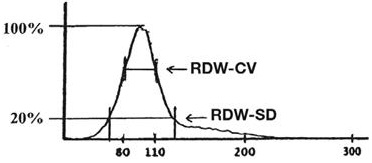
Average concentration of haemoglobin in red cells. - Red cell histogram
Graphical display of variation in erythrocyte volume. - RDW
Measure of variation in erythrocyte volume, calculated from the width of the histogram at 1 SD from the mean, divided by the MCV.
Abnormalities
Abnormal findings include:
Some abnormal findings are specific to blood smears, others are detected on automated analysers.
Splenic macrophages remove damaged and abnormal erythrocytes from circulation; asplenic patients may therefore accumulate a significant number of the more abnormal forms that are produced in small numbers in health.
- Macrocytosis (Normal: 80-10 fL)
Enlarged erythrocytes, occurring usually due to abnormal development or membrane composition. Causes are divided into:- Common:
- Vitamin B12 deficiency
- Folate deficiency
- Alcoholism
- Myelodysplasia
- Uncommon
- Reticulocytosis
- Liver disease
- Hypothyroidism
- Multiple myeloma
- Aplastic anaemia
- Leukaemia
- Drugs
- Common:
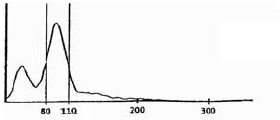
- Dimorphic population
Bimodal distribution of erythrocyte cell volume on a red cell histogram. Usually occurs due to:- Normocytic normochromic cells that existed either prior to disease onset or after treatment
- Microcytic hypochromic cells that existed either prior to (e.g., iron infusion) or after (e.g. myeloablation) treatment
- Sickle Cell
Erythrocyte deformed by HbS which has polymerised under hypoxic stress. Diagnostic of sickle cell disease.
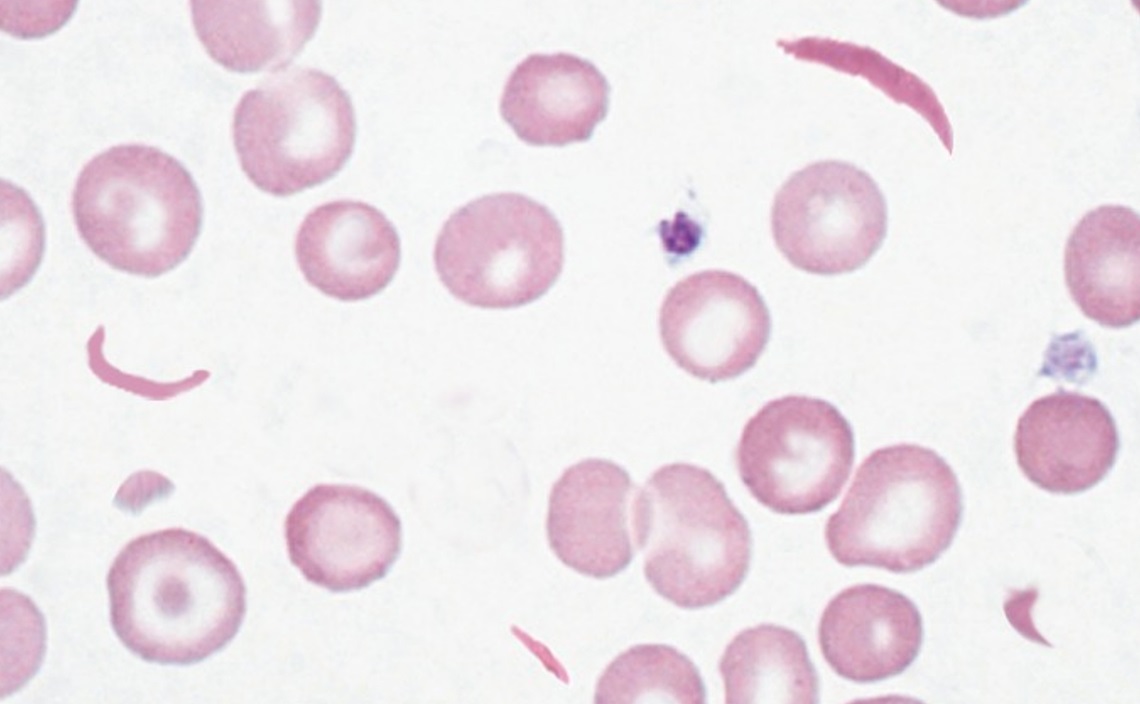
Sickle cell disease is covered under Sickle Cell Disease.
- Reticulocytosis (Normal: 0.5-2.5%)
Juvenile erythrocytes that contain RNA remnants and ribosomes but no nucleus, ejected into circulation in response to anaemia.
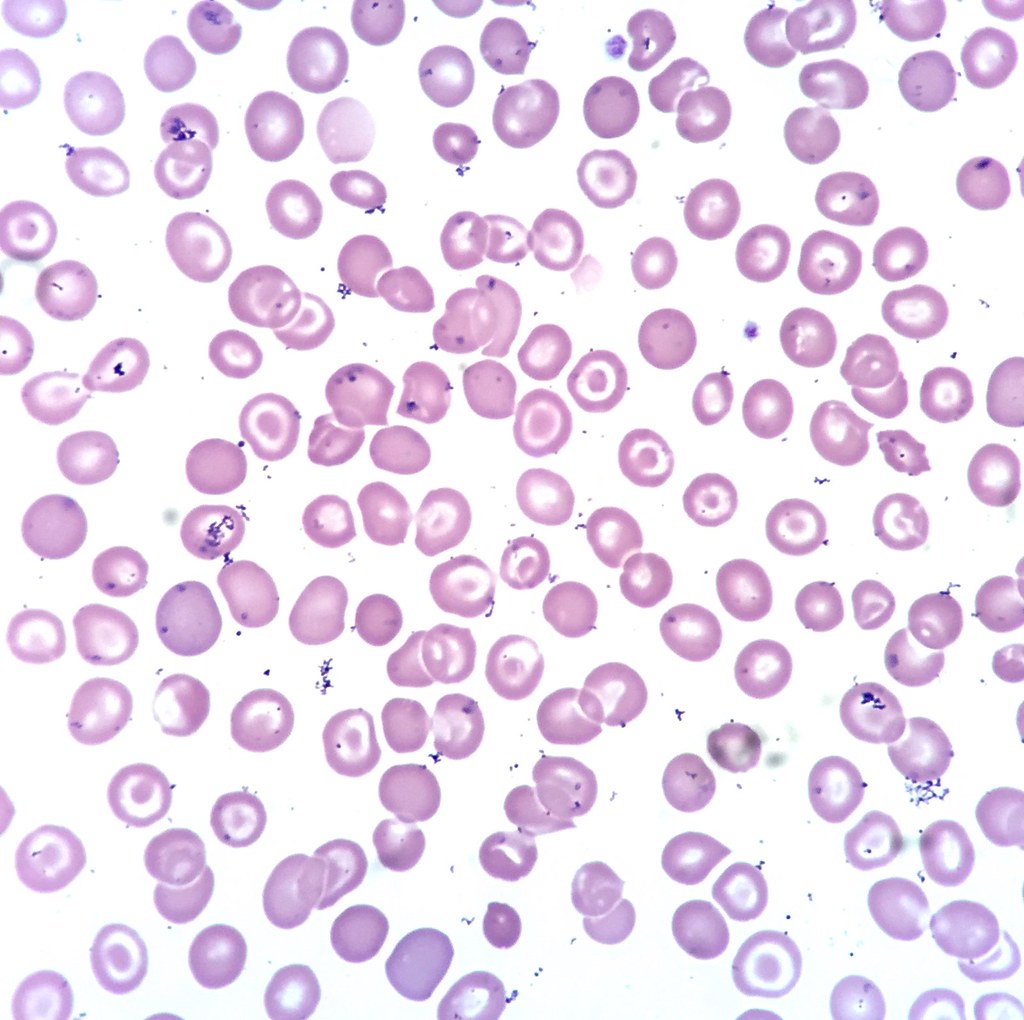
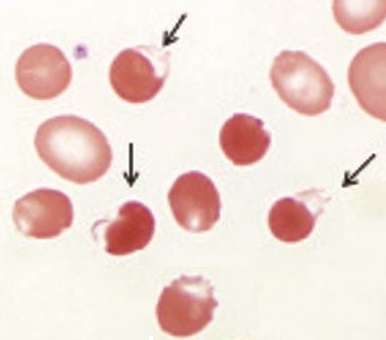
- Schistocytes
Fragmented, irregular, jagged erythrocytes formed by mechanical destruction during haemolysis.
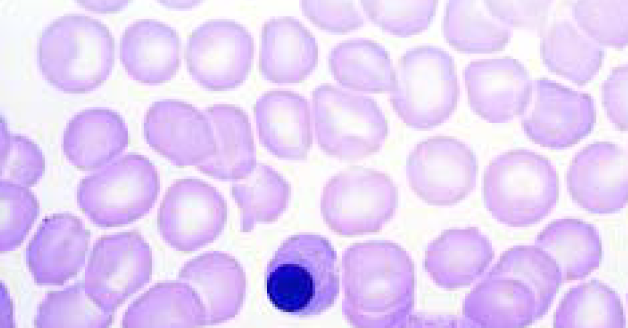
- Nucleated erythrocytes (Normoblastaemia)
Circulating erythrocyte precursors that have yet to eject their nucleus, indicating either:- ↓ DO2
Release of immature red cells to try and add some additional oxygen carrying capacity. Causes include:- Hypoxaemia
- Anaemia
Any cause.
- Hyposplenism
Normoblasts are normally removed in the spleen.- Hyposplenism
- Malaria
- Sickle cell anaemia
- Physiologic
3-10 normoblasts per 100 WBC are normal at birth.
- Bone marrow stress
Upregulation of bone-marrow production, overwhelming capacity of spleen for elimination.- Bone marrow destruction
- Haematological malignancy
- Bony metastases
- Histiocytosis
- Sarcoidosis
- Extramedullary haematopoiesis
- Chronic haemolysis
- Polycythaemia vera
- Bone marrow destruction
- Multifactorial
- Sepsis
- Uraemia
- Liver disease
- DKA
- IBD
- Burns
- Chemotherapy
- ↓ DO2
Hyperviscosity syndrome describes impaired blood flow and organ perfusion due to ↑ blood viscosity, which occurs due to ↑ concentration of cells or macromolecules, and is characterised by:
- Hypervolaemia
- Visual disturbances
- Neurological dysfunction
Coma, seizures.
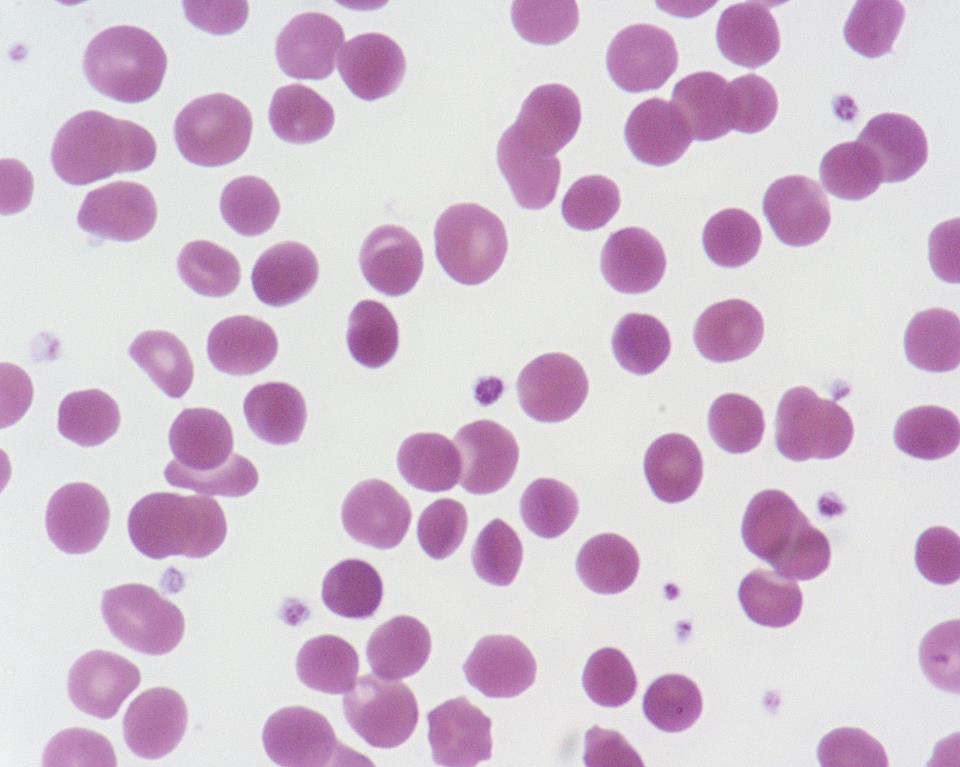
- Rouleaux Formations
Reversible agglutination of erythrocytes in a stack or coin-like formation, which may occur due to:- ↑ Plasma protein (but not albumin)
- Multiple myeloma
- Inflammation
- Malignancy
- Infection
- Inflammation
- ↑ Blood viscosity
- Hyperviscosity syndromes
- Dehydration
- ↑ Plasma protein (but not albumin)

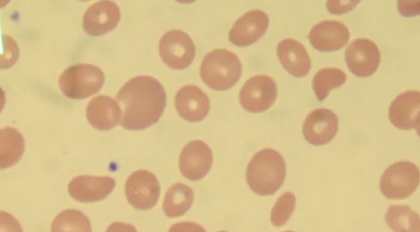
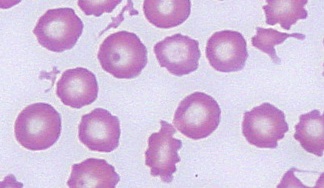
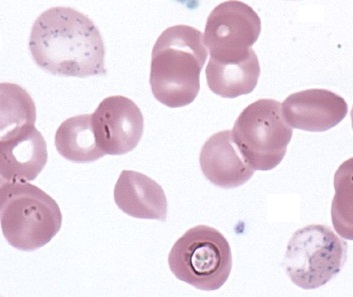
- Target Cells
Erythrocyte with a disproportionate amount of membrane to haemoglobin, and is:- Common in:
- Thalassaemia
- Jaundice
- Post-splenectomy
- Uncommon in:
- Sickle cell anaemia
- Iron deficiency
- Common in:
- Spherocytosis
Erythrocyte with a disproportionate amount of haemoglobin to membrane, resulting in distortion of the biconcave disk to a spherical shape with a greater volume-to-surface area ratio. Causes include:- Haemolytic anaemias
- Hereditary spherocytosis
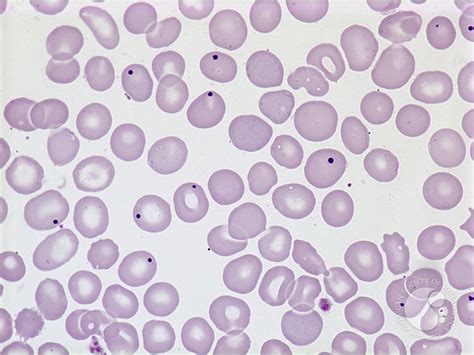
- Howell-Jolly Bodies
Erythrocyte containing DNA remnants, which occur with:- Post-splenectomy
- Haemolysis
- Megaloblastic anaemia
- Macrocytosis
- Corticosteroids
- Pernicious anaemia
- Heinz Bodies (Heinz-Ehrlich bodies)
Erythrocyte containing denatured haemoglobin, indicating oxidative stress due to:- Toxins
- Quinidine
- Primaquine
- Unstable haemoglobin form
- α-thalassaemia
- Methaemoglobinaemia
- Damaged RBC metabolism
- G6PD
- Bactrim toxicity
- Toxins
The pathology of methaemoglobinaemia is covered under Methaemoglobinaemia.
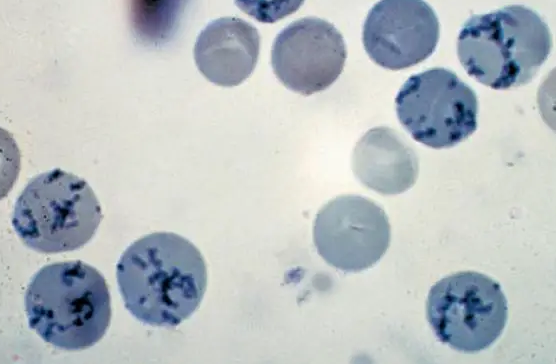
- Basophilic Stippling
Erythrocyte with small blue-staining granules consisting of aggregated ribosome and ribosomal RMA fragments. Associated with:- Lead poisoning
Prevents degradation of ribosomal RNA. Causes include:- Post GSW
- Adulterated drugs
Classically opium. - Contaminated herbal medications
- Heavy metal poisoning
- Lead poisoning
References
- Constantino BT. The Red Cell Histogram and The Dimorphic Red Cell Population. Laboratory Medicine. 2011;42(5):300-308. doi:10.1309/LMF1UY85HEKBMIWO
- Constantino BT, Cogionis B. Nucleated RBCs—Significance in the Peripheral Blood Film. Laboratory Medicine. 2000;31(4):223-229. doi:10.1309/D70F-HCC1-XX1T-4ETE
- Sanchez JR, Lynch DT. Histology, Basophilic Stippling. In: StatPearls. StatPearls Publishing; 2023. Accessed August 7, 2023.