Cardiac Disease in Pregnancy
- Risk of pregnancy depends on specific disease and patients condition, individual counselling by experts is recommended
- Risk stratification is important, and even the lowest-risk patients still have up to 5% risk of peripartum
Pregnancy is a:
This describes the general management of the pregnant patient with cardiac disease. Management of peripartum cardiomyopathy is covered under Peripartum Cardiomyopathy.
- Significant circulatory burden
Achieving a term pregnancy demonstrates presence of physiological reserve. - Time where previously asymptomatic underlying cardiac disease is unmasked and diagnosed
Epidemiology and Risk Stratification
Risk stratification can use:
- Risk prediction model
Provides good general-purpose stratification for patients who may have very individual disease, and a spread of functional stratifications within their lesion.- ZAHARA
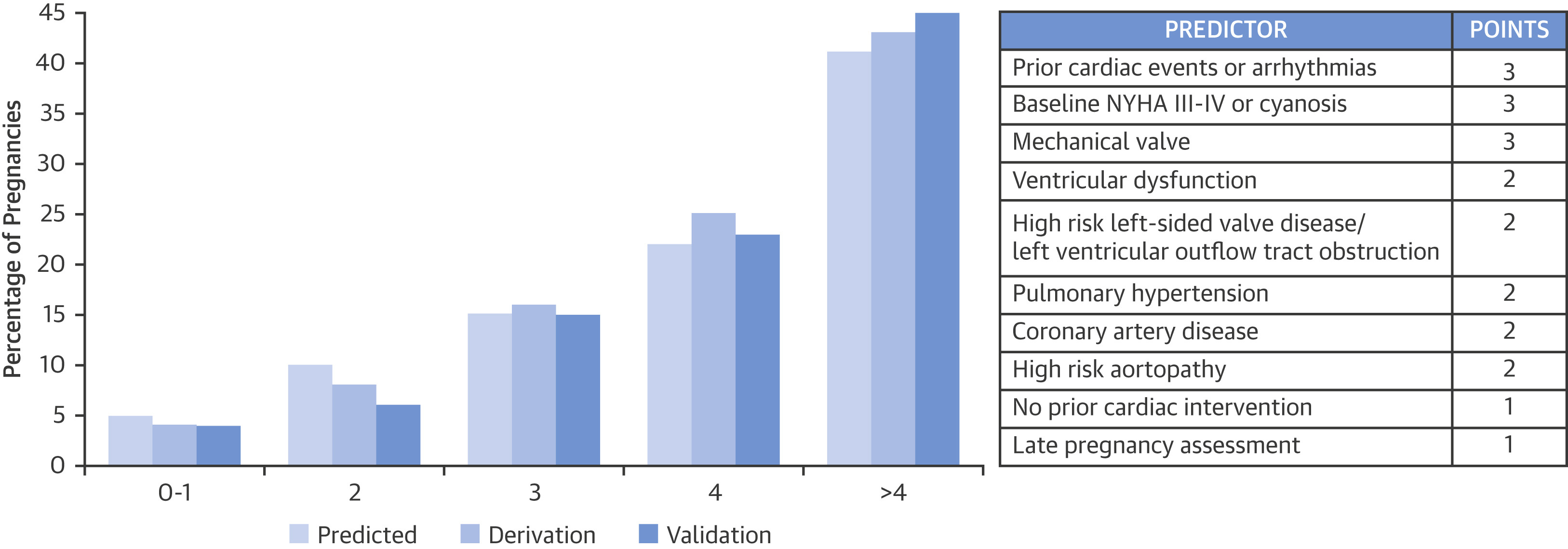
- CARPREG II
- WHO Classification
Comprehensive but may be less useful as does not stratify lesions by severity of that individuals pathology.
CARPREG II
Predictors:
- General
- Prior cardiac events
Includes:- Failure
- Stroke or TIA
- Arrhythmias
- NYHA III/IV or resting SpO2 <90%
- High-risk valve LVOT/ obstruction
- Mild or greater systemic ventricular dysfunction
- No previous cardiac intervention
- Prior cardiac events
- Lesion-specific
- Mechanical valves
- High-risk aortopathies
- Pulmonary hypertension
- Coronary artery disease
- Care related
- Late pregnancy assessment
WHO Risk Stratification
Low (WHO I) risk:
- Cardiology followup limited to one or two visits
- Includes:
- Uncomplicated or mild:
- PS
- PDA
- MV prolapse
- Repaired lesions
- Isolated ectopics
- Uncomplicated or mild:
Moderate (WHO II) risk:
- Require cardiology followup every trimester
- Includes:
- Uncorrected ASD or VSD
- Repaired ToF
- Most arrhythmias
Moderate-severe (WHO II-III) risk:
- Classification depends on individual presentation
- Includes:
- Mild LV dysfunction
- HCM
- Valvular heart disease that is not WHO I or WHO IV
- Repaired coarctation
Severe (WHO III) risk:
- High risk of complications requiring at least monthly cardiology and obstetric review
- Mechanical valve
- Systemic RV or Fontan
- Cyanotic heart disease
- Other complex congenital heart disease
- Aortic dilatation:
- 40-45mm in Marfan’s
- 45-50mm with bicuspid AV
Contraindications to Pregnancy
These patients are also classified as Critical (WHO IV) risk.
Pregnant women who will not consider termination require at least monthly review.
- Severe Pulmonary Hypertension
Mortality up to 50%.
- Severe LV dysfunction
NYHA III-IV or LVEF <30%. - Previous peripartum cardiomyopathy
- Severe obstructive cardiac disease
- HOCM
- Symptomatic Aortic stenosis
- Mitral stenosis
- Pulmonary stenosis
- Unrepaired coarctation
- Aortic dilatation:
- ⩾45mm in Marfan’s
- ⩾50mm with bicuspid AV
- Severe coarctation
Pathophysiology
Key conditions:
- Mitral stenosis is the most common lesion in the pregnant patient
Poorer prognosis with decompensated disease, i.e.:- AF
May precipitate cardiac failure. - Pulmonary hypertension
- May be treated with percutaneous commissurotomy
- AF
- Marfan’s syndrome
- Aortic dissection
Very high risk due to hyperdynamic circulation. - Requires monthly echocardiography
- Aortic root dilatation >50mm strongly consider delivery
- Vaginal delivery possible if aorta <40mm
Risk of straining leading to dissection.
- Aortic dissection
- Pulmonary Hypertension
- Highest risk is in the week following delivery
Consequences:
- Neonate
Complications occur in 20-38% of women with cardiac disease, with key risk factors:- NYHA >II
- Maternal LVOT obstruction
- Smoking
- Multiple gestation
- Use of oral anticoagulants
- Mechanical valve
Clinical Manifestations
Assessment aims are to determine level of function:
- Exercise tolerance
- HR, BP, and SpO2
- Medical therapy
With particular attention to:- Amiodarone
- Warfarin
- ACE-I/A2RBs
Investigations
Key investigations include:
- Bloods
- Haemoglobin
- Coagulation status
- ECG
- Echocardiogram
For any pregnant patient with new or changing symptoms - Cardiac MRI
Management
Highly complicated patients with extensive preparation required:
- Multidisciplinary approach
- Anaesthesia
- Obstetrics
- Maternal-foetal medicine
- Obstetric cardiology
- Intensive care
- Neonatology
- Tertiary centre
- Adult ICU available
- Optimise underlying cardiac disease
Specific Therapy:
- Procedural
- Delivery
Generally planned for between 28-34 weeks.- Vaginal delivery
- Preferred in:
- Severe hypertension
Aim for a “stress free” labour. - Early epidural is recommended
Beware the fixed cardiac-output state.
- Severe hypertension
- Avoid in:
- Aortic dissection
- Marfan’s syndrome with severe aortic root dilatation
- Preferred in:
- Caesarian delivery:
- Aortic dilation >45mm
- Severe AS
- Pre-term labour on anticoagulants
- Eisenmenger’s syndrome
- Severe heart failure
- Vaginal delivery
- Delivery
Anaesthetic Considerations
- C
- Nature of lesion
- Shunts
Required SpO2 and ETCO2. - Air embolisation
- Shunts
- Vascular access
- Circulation goals
- Enhance pulmonary flow
- Optimise CO
- Optimise oxygenation
- Nature of lesion
- D
- Anaesthetic technique
- Regional
- Advantages
- Partner in room
- Avoids risks of GA
- Allows slow titration of anaesthetic
CSE or epidural. - Better post-operative analgesia
- Reduced blood loss
- Reduced PONV
- Disadvantages
- Partner in room
- Anticoagulation
- Maternal anxiety
Subsequent CVS effects. - Complications of regional
- Cannot give 100% oxygen
- Advantages
- General
- Advantages
- Controlled situation
- Reliable
- Anticoagulation status not relevant
- Reduced maternal anxiety
- Easier invasive vascular access
- Facilitate cardiopulmonary bypass or ECMO
- Disadvantages
- Airway and ventilation risks
- Haemodynamic perturbation
Especially at intubation and extubation. - Effect of anaesthetic agents
- Negative inotropy
- Cardiac conduction abnormalities
- Reduced SVR
- Tocolysis
- Risk of awareness
- Greater blood loss
- Poorer post-operative analgesia, PONV
- Advantages
- Regional
- Anaesthetic technique
- I
- Endocarditis prophylaxis
Required in the setting of:- Unrepaired cyanotic CHD
- Repaired CHD with prosthesis
In first 6 months. - Repaired CHD with residual defects
- Endocarditis prophylaxis
The technique chosen will usually come down to the risk-benefit evaluation of the patient, and the skill and preference of the team.
Complications
Consequences of cardiac disease in pregnancy include:
- Maternal
- Death
- C
- Arrhythmias
- Heart failure
Uterine contraction results in mobilisation of uterine blood volume that may precipitate fluid overload.
- D
- CVA
- H
- Embolism
- Foetal
- Death
- SGA
- Prematurity
Prognosis
References
- Endorsed by the European Society of Gynecology (ESG), the Association for European Paediatric Cardiology (AEPC), and the German Society for Gender Medicine (DGesGM), Authors/Task Force Members, Regitz-Zagrosek V, et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: The Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). European Heart Journal. 2011;32(24):3147-3197. doi:10.1093/eurheartj/ehr218