Leptospirosis
Acute febrile illness caused by Leptospira bacterial species, with a range of clinical presentations from:
- Mild influenza-like illness
Occurs early during the leptospiraemia phase, which typically ends after one week as developing antibody response clears bacteraemia. - Icteric leptospirosis (Weil’s disease)
Onset usually at the beginning of the leptospiruria phase.- Combination of:
- Acute liver failure
- Coagulopathy
- AKI
- 5-15% mortality
- Combination of:
- Leptospirosis Pulmonary Haemorrhage Syndrome
- Respiratory symptoms:
- Cough
- Fever
- Pulmonary haemorrhage
- ARDS
- Generally occurs at day 4-6
- Unrelated to degree of liver dysfunction
- 30-70% mortality
- Respiratory symptoms:
Epidemiology and Risk Factors
Globally important public health disease:
- ↑ With climate change
- Cases relate to:
- Flooding
- Rodent-borne transmission
- Occupational exposure related to agriculture, particularly rice farming
- Water sports
- Adventure tourism
Pathophysiology
Leptospira spp. are a family of spirochetes that:
- Infect the PCT
- Are excreted in urine
- Transmitted by exposure to contaminated water or soil
Aetiology
Clinical Features
Following a 5-14 day incubation period:
- Leptospiraemia phase
Typically lasts ~7 days.- Specific
- Myalgia
- Calves
- Lumbar
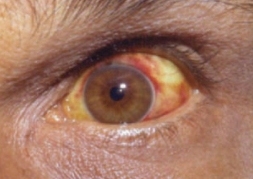
- Conjunctival suffusion
Redness without exudate.
- Myalgia
- Non-specific
- Fever
- Headache
- Retro-orbital pain
- Photophobia
- Myalgia
- Vomiting
- Specific
- A brief intermission of 1-3 days
- Leptospiruria phase
Severe disease occurs:- Weil’s disease
- Pulmonary haemorrhage syndrome
- Cardiomyopathy
- Aseptic Meningitis
Rarely.
Uncommon features include:
- Lymphadenopathy
- Hepatosplenomegaly
- Rash
Rarely:
- Meningism
Diagnostic Approach and DDx
Common differentials:
- Dengue
- Malaria
- Scrub typhus
Investigations
Stain poorly with common stains; dark-field microscopic examination of blood, urine, CSF, or other fluids (dialysate!) are diagnostic.
Bedside:
Laboratory:
- Blood
- LFTs
- FBE
- Variable WCC
- Thrombocytopenia in severe disease
- Cultures
During the first few days of disease, whilst leptospiraemia persists. May take up to 14 days to develop. - Microscopic Agglutination Testing
Diagnostic at 5-7 days. Logistically laborious. - DNA PCR
Diagnostic, limited by access.
- Urine
- Proteinuria
- Pyuria
- Microscopic haematuria
- Cultures
During the first week, during leptospiruria phase.
- CSF
- Leukocytosis
- ↑ Protein
- Normal glucose
Imaging:
Other:
Management
Specific therapy:
- Pharmacological
- Antimicrobials
- 1st line: Benzylpenicillin
- 2nd line:
- Ceftriaxone
- Doxycycline
- Antimicrobials
- Procedural
- Physical
Supportive care:
Disposition:
Preventative:
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
- Death
- F
- AKI
- I
- Jarisch-Herxheimer reaction
Transient acute inflammatory reaction due to release of bacterial toxin and cytokines due to rapid genocide of spirochetes, and can lead to distributive shock, high fever (38-41°C) and occasionally DIC.
- Jarisch-Herxheimer reaction
Prognosis
Key Studies
References
- Toyokawa T, Ohnishi M, Koizumi N. Diagnosis of acute leptospirosis. Expert Review of Anti-infective Therapy. 2011 Jan;9(1):111–21.
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.