External Ventricular Drain
An EVD is a catheter inserted via a burr hole into the right or left lateral ventricle, in order to:
- Drain CSF
- Measure ICP
- Administer medication
EVDs are usually inserted:
- Anteriorly
- Into the non-dominant hemisphere
Indications
Diagnostic and therapeutic:
Contraindications
Anatomy
Equipment
The components of the EVD from proximal to distal are:
- Multi-stage access catheter
Inserted into the ventricle. - Patient connection line
Connects the drain to the monitoring and drainage apparatus. - 3-way stopcock
Allows line to be:- Transduced
A non-flushing pressure transducer should be used, so the line cannot be inadvertently flushed into the brain. - Drained
Note that the EVD cannot simultaneously transduce ICP and drain CSF. When draining, the ICP waveform should transduce the drainage height. - Sampled
Attaching a 3mL syringe allows aspiration of CSF for sampling. Routine sampling ↑ the risk of ventriculitis.
- Transduced
- Drip chamber
A small chamber with volume markers. This chamber:- Can be adjusted relative to the pressure scale
This allows the drainage height (pressure) to be selected.- When ICP exceeds the drainage height, CSF will vent from the EVD
- Standard drainage height is 10-15cmH2O
Many scales provide options for both mmHg and cmH2O.
- Collects CSF
Allows hourly volumes vented to be measured. - Can be periodically emptied into a drainage bag
- Can be adjusted relative to the pressure scale
- Drainage bag
Collects CSF that is vented from the drip chamber.
1mmHg is ~1.3cmH2O; 1cmH2O is ~0.7mmHg.
Technique
Setup and Maintenance
Position and set up:
- The pressure scale should be set at 0 relative to the:
- EAM in a supine patient
This is level with the Foramen of Munro. - Bridge of nose in a lateral patient
- EAM in a supine patient
- The EVD should be clamped prior to moving to prevent CSF over-draining
This includes raising or lowering the bed, transport, physiotherapy, etc. - The EVD should be re-leveled after each position change
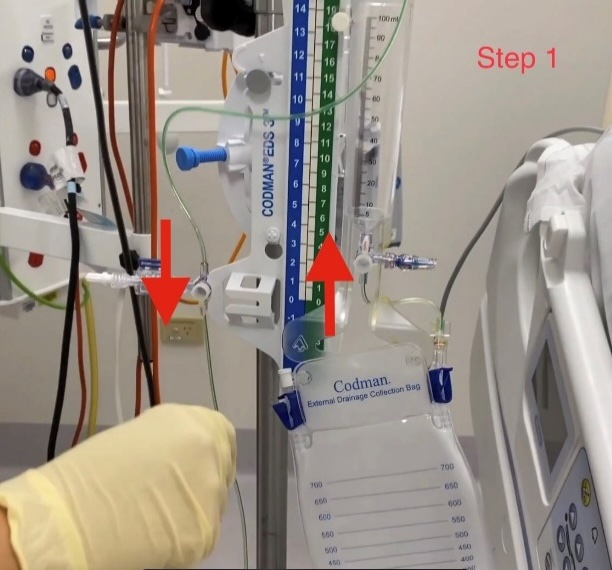
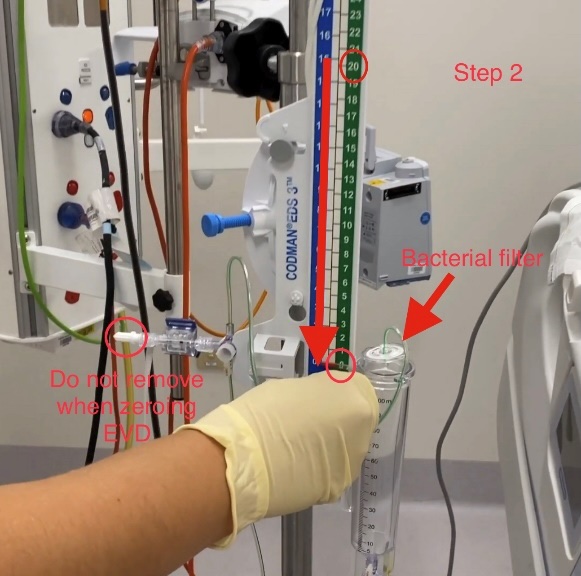
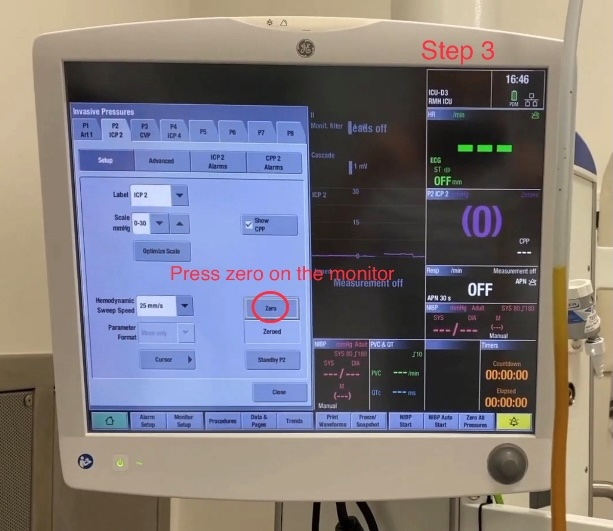
Zeroing:
Do not remove the bung on the transducer - the zero should happen without the system opening to the atmosphere.
- Check EVD is level with the tragus
- Turn the 3-way tap off to patient
This is the tap at the level of the transducer, such that the transducer is ‘open to the drip chamber.’ - Drop level of the drip chamber to 0
- Zero pressure on monitor
- Return trip chamber to desired height
- Close 3-way tap to the transducer

Therapeutic Use
The EVD will generally be set in one of two modes:
Continuous drainage is used for hydrocephalus (and in SAH, to prevent hydrocephalus); intermittent venting is used in TBI.
- Continuous drainage
- EVD is left open at a set height
CSF will passively drain when ICP > set height.- EVD ‘weaning’ may be performed by raising the set height - absence of CSF drainage indicates that ICP is not rising above this level
- High-volume CSF drainage is >30mL/hr
Nursing notification should occur if EVD drainage is >20mL/hr. - The EVD is generally not transduced in these circumstances, although it is good practice is to transduce every hour to confirm patency if there has been no CSF drainage
A pressure transducer may not need to be attached if the EVD is being used in this way.
- EVD is left open at a set height
- ICP monitoring/intermittent venting
- Continuously transduced
Intermittently vented in case of ↑ ICP.
- Continuously transduced
Other uses:
- CSF sampling
CSF may be sampled from an EVD, generally to evaluate for the presence of ventriculitis. - Medication administration
Occasionally, medications (e.g. thrombolytics) are administered through an EVD.
Troubleshooting
- Blocked EVD
- EVDs can become blocked with blood or other exudate
- Briefly lowering the EVD (‘dropping to the floor’) will detect blockage as CSF should flow under gravity when the EVD is lowered
This should be done only for a few seconds to confirm CSF flow, over-draining should be avoided to prevent collapse of the ventricles and intracranial haemorrhage. - A blocked EVD may be flushed to restore patency, and should be done by the neurosurgeon.
Complications
- I
- Ventriculitis
Risk is ↑ with:- Non-sterile insertion
- Duration of EVD insertion
- SAH/IVH present
- Skull fracture
- Frequent CSF sampling
- Ventriculitis
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.