Tracheostomy Overview
Definitive airway produced by inserting a tube subglottically through the anterior neck directly into the trachea. May be:
This covers the management of a tracheostomy, including considerations for their use. Tracheostomy weaning and insertion of percutaneous tracheostomy are covered elsewhere.
- Surgical
Dissection and incision of the trachea under direct vision. - Percutaneous
Seldinger dilation.
Indications
| Favours Percutaneous | Favours Surgical |
|---|---|
| ↓ Bleeding | Vascular insertion site on ultrasound |
| ↓ Infection | Complex neck anatomy |
| ↓ Tracheal stenosis | Less risk of death/cardiac arrest |
| Better cosmetic result | Greater airway backup (anaesthetist/surgeon) |
| Logistics (no waiting on surgical lists) | Does not require bronchoscope |
| No risk of intrahospital transfer | Emergent |
- A
- Surgical
e.g. Laryngectomy.
- Surgical
- B
- Long-term mechanical ventilation
Useful for patients requiring long-term ventilation, and to aid respiratory weaning by:- ↓ Sedation requirements
Facilitates spontaneous ventilation, ↑ proportion of respiratory work done by the patient. May lead to ↓ total time on mechanical ventilation. - ↓ Work of breathing
↓ Airway resistance and (marginally) ↓ dead space relative to ETT. - ↓ Airway trauma
↓ Risk of laryngeal stenosis, vocal cord ulceration, and improves voice recovery. These risks rise after 1 week of oral intubation. - ↓ Aspiration risk
Glottic competence is restored, so the tube cuff is not the only thing preventing aspiration. - Better secretion management
Awake patients can cough more effectively. Potentially less VAP. - Better oral care
Can brush teeth.
- ↓ Sedation requirements
- Long-term mechanical ventilation
- D
- ↓ Sedation requirements
Better tube tolerance and patient comfort compared to oral ETT.- Improved communication
- Desedation facilitates interaction
- Lip-reading
Easier without an ETT. - Talking
With the cuff down, and with or without a speaking valve. Requires generating subglottic pressure of >2cmH2O.
- Facilitate neurological assessment
- Improved communication
- Quality of life
- ↓ Sedation requirements
- E
- Facilitate physiotherapy
Positioning, rehabilitation, coughing.
- Facilitate physiotherapy
Considerations
Considerations for tracheostomy insertion include:
Timing of tracheostomy insertion is difficult. In general:
- Clinicians are bad at predicting who will need a tracheostomy
- Routine early tracheostomy therefore leads to large numbers of unnecessary tracheostomies
- An approach:
- Early if prolonged ventilation inevitable
e.g. GBS. - >10 days following mechanical ventilation, without imminent extubation
- Early if prolonged ventilation inevitable
- A
- Neck anatomy
- Vascularity
- Length of accessible trachea
Patients without much extra-thoracic trachea will be more difficult with both insertion and management.
- Intubation grade
- C-spine stability
- Neck anatomy
- B
- Respiratory function
Ideally:- FiO2 <0.6 Risk of airway fire with electrocautery, and indicates tolerance of interruption of ventilation during insertion.
- PEEP <10cmH2O Tolerance of de-recruitment and interruption of ventilation during insertion.
- Respiratory function
- H
- Coagulopathy
- I
- Infection
At site of insertion.
- Infection
Components
Components of the tracheostomy setup:
- Tracheostomy tube
May be:- Fenestrated
Tube has holes above the cuff.- Permits coughing, phonation, and aspiration
Outer portion needs to be blocked to divert gas flow via vocal cords. - Aids respiratory weaning
- Patient must protect own airway
- Improves swallow
- Inner cannula can be:
- Fenestrated
Allows tube to function as a fenestrated tube. - Unfenestrated
Blocks fenestration, which permits mechanical ventilation. Mechanical ventilation of a fenestrated tube results in significant circuit leak and a distressed, continually-exhaling patient.
- Fenestrated
- Permits coughing, phonation, and aspiration
- Unfenestrated
- Fenestrated
- Inner cannula
Inner tube placed inside the tracheostomy tube to prevent it being contaminated.- Easy cleaning
Just remove the inner cannula, clean, and replace. - ↓ Internal dimensions/↑ airway resistance
Degree depends on the catheter size.
- Easy cleaning
- Speaking (Passy Muir) valve
One-way valve that allows a patient to inspire through the tracheostomy, and then expire via the native away, allowing phonation. The valve:- Requires the cuff to be deflated
Or the patient will be unable to exhale. - A humidifier can (and should) be used
An HME will be ineffective as the patient exhales via a different route. - Can be used with or without a ventilator
The ventilator will need to be set accordingly, to prevent continual alarms.
- Requires the cuff to be deflated
- Tracheostomy cap
Occlusive cover for the tracheostomy tube, preventing inspiration via the tracheostomy tube, turning the tube into a partial upper airway obstruction. This requires the patient to inspire and expire via the native airway, and also the cuff to be deflated.
Management
Caring for a tracheostomy tube:
Tracheostomy patients are high risk and should be managed by trained staff. An ICU outreach team is beneficial.
- A
- Cuff pressures
Keep <30mmHg to reduce the risk of tracheal ulceration and stenosis. - Cleaning
Inner cannula (if present) should be cleaned when necessary. - Suctioning
- Shallow tracheal suctioning (to the length of the tube) to remove secretions, particularly if cough is inadequate
- Suction channels (above the cuff) should be suctioned at least Q4H
- Wound care
The wound must be kept clean to prevent infection.
- Cuff pressures
- B
- Humidification
Should be routine, including if patient is using trache hood or Swedish nose. Important for:- Patient comfort
- Secretion management
↓ Viscosity.
- Humidification
Facilitating Speech
Speech greatly improves the quality of life of a patient with a tracheostomy. All methods of phonation require gas to be exhaled via the native airway.
Contraindications to speaking:
- High aspiration risk
- Unconscious/comatose
- Loss of upper airway reflexes
- High secretion load
- Unable to exhale via native airway
- Upper airway obstruction
- Inadequate lung mechanics
↑ Resistance, ↓ compliance.
| Approach | Considerations | Advantages | Disadvantages | |
|---|---|---|---|---|
| Cuff down, with: | Nothing else |
|
|
|
| Finger occlusion |
|
|
||
| Speaking valve |
|
|
|
|
| Cuff up, with: | Fenestrated tracheostomy |
|
|
|
| Above cuff vocalisation |
|
|
|
|
Combining a fenestrated tube and a speaking valve significantly prolongs expiration time, which may ↑ FRC and prevent small airway collapse.
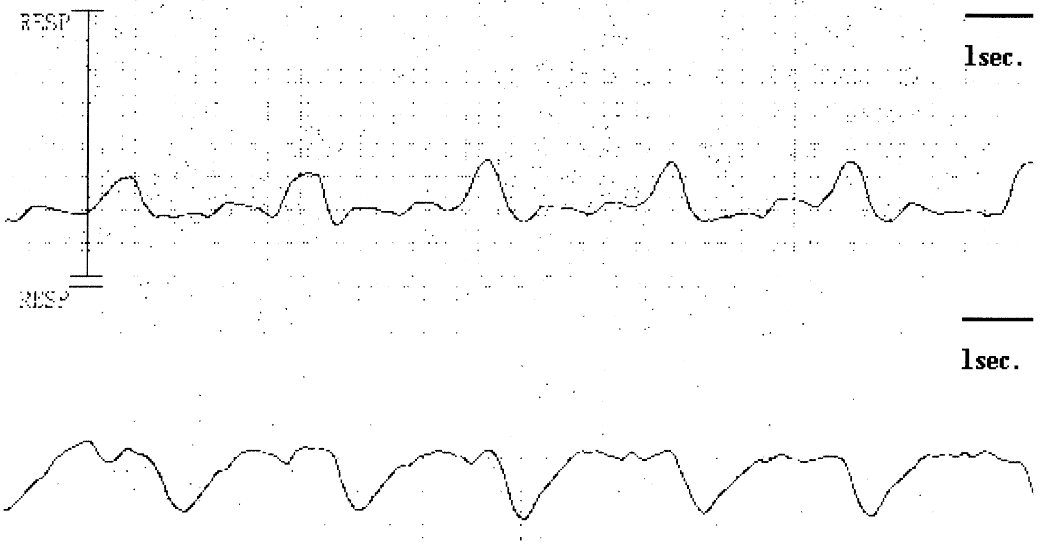
Electrographic chest wall movement:
- Top: Standard tracheostomy tube
- Bottom: Fenestrated tube with speaking valve
Complications
In-situ tracheostomy:
- A
- Dislodgement
Risks include:- Patient
- Agitation
- Large s
- Equipment
- Poorly sized tube
- Staff
Inadequate:- Training
- Numbers
- Patient
- Bleeding
~5% of cases.- Early
Bleeding within 48 hours is likely venous. - Late
Due to erosion of the tracheostomy into a vascular structure.- Tracheo-innominate fistula
Erosion (classically of the cuff) into the innominate artery.- Leads to catastrophic:
- Bleeding and airway soiling
- Air entrainment
- Leads to catastrophic:
- Any bleeding between 3 days and 6 weeks should be investigated for a fistula
Either bronchoscopically or via CT.
- Tracheo-innominate fistula
- Early
- Obstruction
- Bleeding
- Secretions
↑ Risk if dehumidified.
- Dislodgement
- B
- Failure to wean
If the patient is unable to wean from the ventilator despite the tracheostomy, this may be an unsatisfactory outcome for both patient and family. - Pneumonia
↑ Risk due to bypass of normal upper respiratory protective mechanisms. Occurs in ~25% of patients.
- Failure to wean
- D
- Quality of life
Generally worse in patients who have received a tracheostomy, compared to patients who did not.
- Quality of life
- G
- Swallowing difficulty
- I
- Infection
Either of the stoma, or contamination of wounds (sternal, CVC) with secretions.
- Infection
Post-tracheostomy:
- A
- Tracheal stenosis
Commonly occurring (1-2%), rarely significant. Risk ↑ with:- Procedural
- Tracheal ring fracture
- Equipment
- Oversized cannula
- Patient
- Male
- Elderly
- Prolonged duration of use
- Procedural
- Tracheomalacia
Loss of tracheal cartilage (usually ischaemic), leading to collapse under negative-pressure inspiration. - Persistent stoma
May require surgical repair.
- Tracheal stenosis
Key Studies
- TRACMAN (2013)
- ~900 intubated Britons on day 4 of intubation whose treating clinician believed they will need ⩾7 further days of mechanical ventilation, and a tracheostomy is not otherwise indicated or contraindicated
- Multicentre, randomised trial
- 80% power for 8.3% ARR ↓ in 30 day mortality (!!), assuming baseline of 31.5%
Multiple readjustments due to changing baseline mortality and recruitment fatigue. - Early (day 4) vs. Late (⩾10 day) tracheostomy
- Early
- 85% received tracheostomy
- 7% never received tracheostomy
- 7.5% received late tracheostomy
- Late
- 40% received tracheostomy after day 10 of admission
- 53% did not receive a tracheostomy as it was no longer indicated
- 7% received tracheostomy before day 10
- Early
- No change in 30 day mortality (30.8% vs. 31.5%)
- No difference in secondary outcomes, including ICU length of stay or ventilated days
- ~6% complication rate
- Overall: We are not successful at predicting need for tracheostomy, there are not insignificant procedural risks, and early tracheostomy does not appear to have benefits in accelerating ventilator weaning
References
- De Leyn, Paul, Lieven Bedert, Marion Delcroix, Pieter Depuydt, Geert Lauwers, Youri Sokolov, Alain Van Meerhaeghe, Paul Van Schil, and Belgian Association of Pneumology and Belgian Association of Cardiothoracic Surgery. “Tracheotomy: Clinical Review and Guidelines.” European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-Thoracic Surgery 32, no. 3 (September 2007): 412–21.
- Dulguerov, Pavel, Gysin, Claudine, Perneger, Thomas, MD, PhD, Chevrolet, Jean-Claude. Percutaneous or surgical tracheostomy: A meta-analysis. Crit Care Med. 1999;27(8):1617-1625.
- Hess, Dean R. “Facilitating Speech in the Patient With a Tracheostomy.” Respiratory Care 50, no. 4 (April 1, 2005): 519–25.
- Ailawadi, Gorav. “Technique for Managing Tracheo-Innominate Artery Fistula.” Operative Techniques in Thoracic and Cardiovascular Surgery 14, no. 1 (March 1, 2009): 66–72. .
- Donaldson, Lachlan, and Raymond Raper. “Successful Emergency Management of a Bleeding Tracheoinnominate Fistula.” BMJ Case Reports 12, no. 12 (December 2019): e232257. https://doi.org/10.1136/bcr-2019-232257.
- Young D, Harrison DA, Cuthbertson BH, Rowan K, for the TracMan Collaborators. Effect of Early vs Late Tracheostomy Placement on Survival in Patients Receiving Mechanical Ventilation: The TracMan Randomized Trial. JAMA. 2013;309(20):2121-2129. doi:10.1001/jama.2013.5154
- McGrath B, Lynch J, Wilson M, Nicholson L, Wallace S. Above cuff vocalisation: A novel technique for communication in the ventilator-dependent tracheostomy patient. Journal of the Intensive Care Society. 2016;17(1):19-26.
- Fukumoto M, Ota H, Arima H. Ventilator weaning using a fenestrated tracheostomy tube with a speaking valve. Critical Care and Resuscitation. 2006;8(2).