Spontaneous Bacterial Peritonitis
Infection of ascitic fluid occurring in absence of any evident infective source, which may present as:
SBP is generally a monomicrobial infection. Multiple organisms suggests secondary peritonitis from faecal contamination, which is a surgical disease.
- Florid sepsis
- Insidious decline
Epidemiology and Risk Factors
Risk factors:
Child-Pugh score is covered under Child-Pugh Score.
- Previous SBP
- Invasive devices
- Hepatic dysfunction
- Child-Pugh Grade C
- Variceal bleeding
- Infection
- UTI
- Intestinal bacterial overgrowth
Pathophysiology
Major factors:
- Ascites is a ready-made, continuously available viable culture medium
- Immunosuppression secondary to chronic liver disease
Aetiology
Causative organisms:
- E. coli: 37%
- K. pneumoniae: 17%
- Other Gram positives: 14%
- S. pneumoniae: 12%
- Other gram negatives: 10%
- S. viridans: 9%
Clinical Manifestations
Features include:
Asymptomatic in ~10%.
- Fever: 70%
- Abdominal pain: 50%
- Tenderness: 40%
- Rebound: 10%
- Confusion
- Altered level of consciousness: 54%
Diagnostic Approach and DDx
Mortality approaches 80% if an unnecessary laparotomy is performed, so it is vital to distinguish SBP from secondary peritonitis.
Key differentials:
- Secondary peritonitis
Indicated by:- Peritonism
- Localising abdominal pain
- Multiple organisms on Gram stain
- Failure of antibiotic therapy
- Ascitic fluid findings
Two of:- Protein >1g/dL
- Glucose <3mmol/L
- LDH > ULN of serum LDH
Investigations
Laboratory:
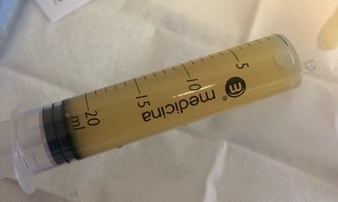
- Ascitic tap
Required for diagnosis.- Usually low bacterial concentrations of a single organism
- Consider using a micropuncture kit (e.g. 21G spinal needle) to ↓ risk of continual leak from puncture site
- 10-20mL should be placed into blood culture bottles to increase yield
- Diagnostic criteria:
- WCC >250/mm3
- Evidence of bacteria
Usually only one.
- Paracentesis should be repeated at 48 hours after microbial therapy
Cirrhotic patients with large volume ascites should be tapped on ICU admission irrespective of their admission diagnosis, as ~10% will be complicated with SBP
Imaging:
- CT
If concern for secondary peritonitis.
Management
- Appropriate antibiotics
- Give 20% albumin
- Cease nephrotoxins and antihypertensives
- Consider repeat paracentesis
Specific therapy:
- Pharmacological
- Antibiotics
Choice is contextual, however:- Ceftriaxone 2g IV daily
- Tazocin 4.5g IV TDS
If resistant species, nosocomial infection, or septic shock.
- 20% Albumin
- 1.5g/kg IV, then 1g/kg 48 hours later
- ↓ AKI
- Substantial ↓ mortality by ↓ hepatorenal syndrome
- Antibiotics
- Procedural
- Repeat paracentesis
At 48 hours to evaluate for treatment failure; unnecessary if organism is susceptible and there is clinical improvement.
- Repeat paracentesis
Supportive care:
- C
- Cease β-blockade
Many patients will be on propranolol for variceal haemorrhage prophylaxis, which will ↓ CO in the septic state.
- Cease β-blockade
- G
- Feeding
- ↓ Bacterial translocation
- Cease PPI
- Rifaximin 400mg PO TDS
- Feeding
Disposition:
- Ongoing prophylactic antibiotics
May be appropriate in high risk patients; agents include:- Rifaximin
- Norfloxacin
- Ciprofloxacin
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
- B
- Pleural effusion
- May occur when there is communication betwen the abdomena nd pleura
- Thoracocentesis is indicated for:
- Respiratory failure
- Clinical suspicion of empyema
- Pleural effusion
Prognosis
Features associated with ↑ mortality include:
- Resistant organism
Key Studies
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.