Clostridioides Difficile
Also known as Clostridium difficle and C. diff.
Clostridium difficile was renamed in 2016, after genetic analysis identified it should fall under the peptostreptococcaceae family, and thus be a Peptoclostridium.
To avoid excessive disruption to the status quo, some microbiological taxonomy loopholes were exploited to forge a new genus Clostridioides, and so keep the familiar C. diff abbreviation.
Infective diarrhoea caused by Clostridioides Difficile that:
- May lead to pseudomembranous colitis
- Occurs secondary to:
- Broad-spectrum antibiotics
- Chemotherapy
Epidemiology and Risk Factors
Causes:
- 10-25% of antibiotic-associated diarrhoea
- Almost all cases of pseudomembranous colitis
Major risk factors include:
- Broad-spectrum antibiotics
- Clindamycin
- Cephalosporins
- Fluoroquinolones
- Immunosuppression
- Severity of illness
- IBD
- Exposure to infected patient
- Age >65
- SUP
PPIs double risk. - Prolonged hospital stay
- Renal impairment
Pathophysiology
Aetiology
Clostridioides Difficile is:
- A spore-forming, Gram positive, anaerobic bacilli
- Toxin-producing
Most bacteria produce both, but up to 25% produce neither:- Toxin A
- Enterocyte-toxic
- Attracts neutrophils
- Toxin B
More potent than B.
- Toxin A
- An extremophile
Resistant to:- Dessication
- Most cleaning products
Notably, not chlorine.
Clinical Features
Two clinical pictures:
- Diarrhoea with associated fever
- Mucoid
- Green-ish
- Watery
- Presence of pseudomembranes
- Ileus (and no diarrhoea) with leukocytosis and toxic megacolon
Assessment
History:
Exam:
Diagnostic Approach and DDx
Features suggestive of C. difficile:
- Characteristic stools
- Watery
- Green-ish
- Mucoid
- >3/24 hours
- 3-9 days after antibiotics
- Previous broad spectrum antibiotics
- Fever
- Abdominal pain
- Distension
- Positive investigations
- AKI
Investigations
Bedside:
Laboratory:
- Blood
- FBE
- Leukocytosis
- LFT
- Hypoalbuminaemia
- FBE
- Stool
- Antigen and toxin PCR
Sensitive, persist after resolution of infection. - Culture
- 2-3 days to grow
- Technically demanding
- Most useful for epidemiological purposes for strain typing
- Antigen and toxin PCR
Imaging:

- AXR
- “Thumbprinting” of bowel
Thickening of haustra due to oedema, leading to an appearance of thumbprints projecting into the aerated colonic lumen at regular intervals. - Pneumoperitoneum
- “Thumbprinting” of bowel
- CT
- Inflamed bowel
- Perforation
- Pneumoperitoneum
Other:
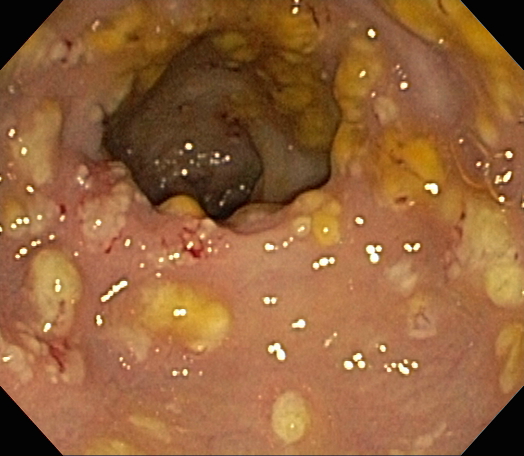
- Proctoscopy/flexible sigmoidoscopy
- Facilitates direct visualisation of pseudomembranes
- Method to detect severe disease
- Risk of perforation limits use
- Role in severe disease and antigen and toxin tests are negative or unavailable
Management
- Standard sepsis management
Covered under Management. - Stop inciting antibiotics
- Oral antibiotics
Empirically if high pre-test probability.
Specific therapy:
- Pharmacological
- Cease other antibiotics
- Oral antibiotics
- Mild-moderate infection
- Metronidazole 500mg PO Q8H for 10 days
Change to fidaxomicin or vancomycin if no response in 5 days.
- Metronidazole 500mg PO Q8H for 10 days
- Severe infection
- Fidaxomicin 200mg PO Q12H for 10 days
Preferable to vancomycin, if available. - Vancomycin 125-500mg PO Q6H for 10 days
- Higher dose indicated in shock
- Can be given via enema if ileus present
In this case the dose is 500mg in 100mL Q6H.
- Metronidazole 400mg IV Q8H for 10 days
In addition to fidaxomicin or vancomycin.
- Fidaxomicin 200mg PO Q12H for 10 days
- Mild-moderate infection
- Bezlotoxumab 10mg/kg
- Antibody against Toxin B
- Indicated in second recurrence
- Single dose of 10mg/kg
- Procedural
- Faecal microbiota transplant
- Justified by restoring colonic microbial biodiversity that was disrupted by the antibiotic-induced genocide
- Indicated for third recurrence
- Risk of infection transmission
- Faecal microbiota transplant
- Physical
- Faecal management system
- Bowel resection
Consider with:- Sepsis
- WCC >50×103/mL
- Lactate >5mmol/L
Supportive care:
- D
- Analgesia
- F
- Correct electrolyte disturbances
Preventative:
- Antimicrobial stewardship
- Appropriate infection control
- Contract precautions
- Soap-and-water handwashing
- Individualise equipment
Marginal and Ineffective Therapies
- Probiotics
Anaesthetic Considerations
Complications
- C
- SIRS
- Hypovolaemia
- F
- Electrolyte disturbances
- G
- Toxic megacolon
- Perforation
- I
- Abdominal sepsis
Prognosis
Poor prognostic features include:
- Age >70
- WCC
- Rate of rise
- Peak >20×103/mL
- Albumin <25g/L
- AKI
- SBO
- Ileus
- Fever >38.0°C
Key Studies
References
- O’Grady NP, Barie PS, Bartlett JG, et al. Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Critical Care Medicine. 2008;36(4):1330.
- Diseases TLI. C difficile—a rose by any other name…. The Lancet Infectious Diseases. 2019;19(5):449. doi:10.1016/S1473-3099(19)30177-X
- Johnson S, Lavergne V, Skinner AM, et al. Clinical Practice Guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 Focused Update Guidelines on Management of Clostridioides difficile Infection in Adults. Clinical Infectious Diseases. 2021;73(5):e1029-e1044. doi:10.1093/cid/ciab549
- Case courtesy of Derek Smith. Thumprinting. Radiopaedia.org, rID: 31329.