Intracerebral Haemorrhage
Bleeding into brain parenchyma, usually from a primary vascular cause.
This discusses “pure” ICH, which most commonly occurs with haemorrhagic stroke.
Pure ICH from aneurysmal bleeding is rare, as the majority have subarachnoid (SAH) or ventricular (IVH) extension. Trauma often causes a variety of intra- and extra-axial bleeds, although isolated contusions are common.
Epidemiology and Risk Factors
Pathophysiology
Haemorrhage:
- Size is a function of the anatomical resistance of the site of bleeding
- Cortical typically larger than pontine
- Degree of dysfunction is determined by the region of brain destroyed
- Pontine typically more disabling than cerebral
Intracranial haemorrhage can be divided into:
- Intra-axial
Intracerebral haemorrhage. - Extra-axial
- EDH
- SDH
- SAH
- IVH
Aetiology
Causes:
- Vascular
- Hypertensive haemorrhage
Prolonged systemic hypertension results in vascular degeneration and formation of microaneurysms, usually at bifurcations. - Aneurysmal
Cerebral aneurysms can occasionally cause ICH without SAH. - AVM
- Microvascular
- Arteriolesclerosis
- Cerebral Amyloid Angiopathy
- Hypertensive haemorrhage
- Trauma
Clinical Manifestations
- Usually no prodrome
- Sudden onset and rapid deterioration with:
- Focal neurology
- Depression of consciousness
- ↑ ICP
Ocular palsies.
Diagnostic Approach and DDx
Key differential diagnoses:
- Ischaemic stroke
Difficult to distinguish clinically in early stages.
Investigations
Bedside:
Laboratory:
Imaging:
Other:
Management
- Limit haematoma expansion
- Reverse anticoagulation
- Control ICP
Resuscitation:
Principles of management are the same as for ischaemic stroke (covered under Stroke), with key differences being:
- More aggressive blood pressure control
- Avoid anticoagulation and thrombolysis
- C
- Hypertension control
Acute ↓ of SBP to 130-150mmHg, ideally within 1 hour.
- Hypertension control
- D
- ICP control
- ICP monitoring
For GCS ⩽8.
Specific therapy:
Reversal of therapeutic anticoagulation is covered in detail under ?sec-anticoag.
- Pharmacological
- Reversal of anticoagulation
- Warfarin
PCC, irrespective of INR. Can be given prior to INR result returning. - Direct Xa inhibitor
- Consider Andexenat alfa
- PCC may be used to improve haemostasis
- Warfarin
- Reversal of anticoagulation
- Procedural
- EVD
Indicated in:- Secondary hydrocephalus
- Intraventricular extension
- EVD
- Physical
Supportive care:
- H
- Platelets
Only for correction of thrombocytopenia or prior to neurosurgical intervention.
- Platelets
Disposition:
Marginal and Ineffective Therapies
- Hyperventilation
↓ PaCO2 to <30mmHg results in ↓ CBF and cerebral ischaemia - Steroids
Anaesthetic Considerations
Complications
Prognosis
Key Studies
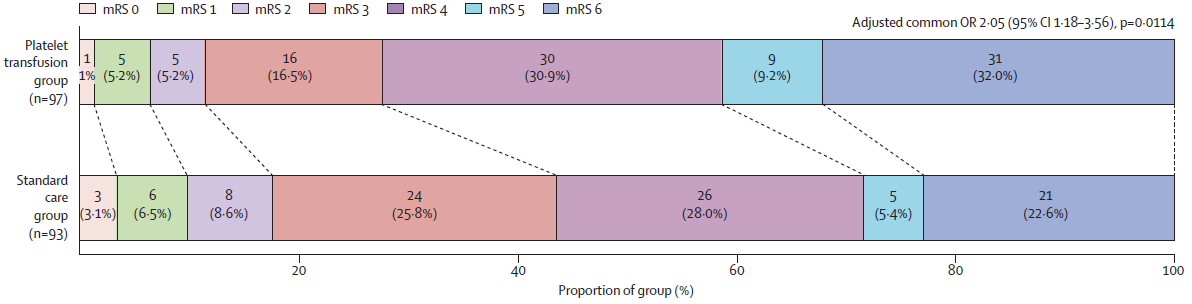
- PATCH (2016)
- 190 European adults on antiplatelet therapy with supratentorial non-traumatic, non-aneurysmal ICH and a GCS from 8-15, without intraventicular haemorrhage, history of coagulopathy
- Multicentre (41), assessor blinded RCT
- 91% power to detect OR of 0.43 (!) between pairs of mRS categories
- Platelets vs. standard care
- Platelets
- 5 units if on COX inhibitor
- 10 units if on ADP receptor inhibitor
- 4 did not receive platelets
- Control
- 2 received platelets
- Platelets
- Worse functional outcome at 3 months (OR ~2, CI 1.2-3.6)
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.
- Baharoglu MI, Cordonnier C, Salman RAS, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. The Lancet. 2016;387(10038):2605-2613. doi:10.1016/S0140-6736(16)30392-0