Maxillofacial Trauma
Combination of facial fractures and soft tissue damage that may be life-threatening due to:
- Haemorrhage
- Airway compromise
- Bleeding
- Oedema
- Can be massive and cause significant distortion
- Generally evolves over 24-48 hours
- Association with significant intracranial injury
Epidemiology and Risk Factors
Associated with:
- Young
Predominantly 15-25. - Male
- Alcohol
Pathophysiology
Mandibular fractures:
- Commonly occur at structurally vulnerable sites, independent of point of impact
- Condyles
May limit mouth opening, even after muscle relaxation. - Symphysis
Point of midline fusion. - Angle
- Condyles
- Multiple fractures are common
Mid-face fractures:
The midface acts similarly to a crumple zone on a car and collapses progressively under impact. Multiple complex facial fractures are therefore the most common presentation.
- Facial skeleton consists of several small compartments supported by three vertical buttresses
- Compartments:
- Orbits
- Nasal cavities
- Paranasal sinuses
- Buttresses:
- Nasomaxillary pillars
- Zygomaticomaxillary pillars
- Pterygomaxillary pillars
- Compartments:
- Fracture-dislocations occur as the facial skeleton collapses around these pillars
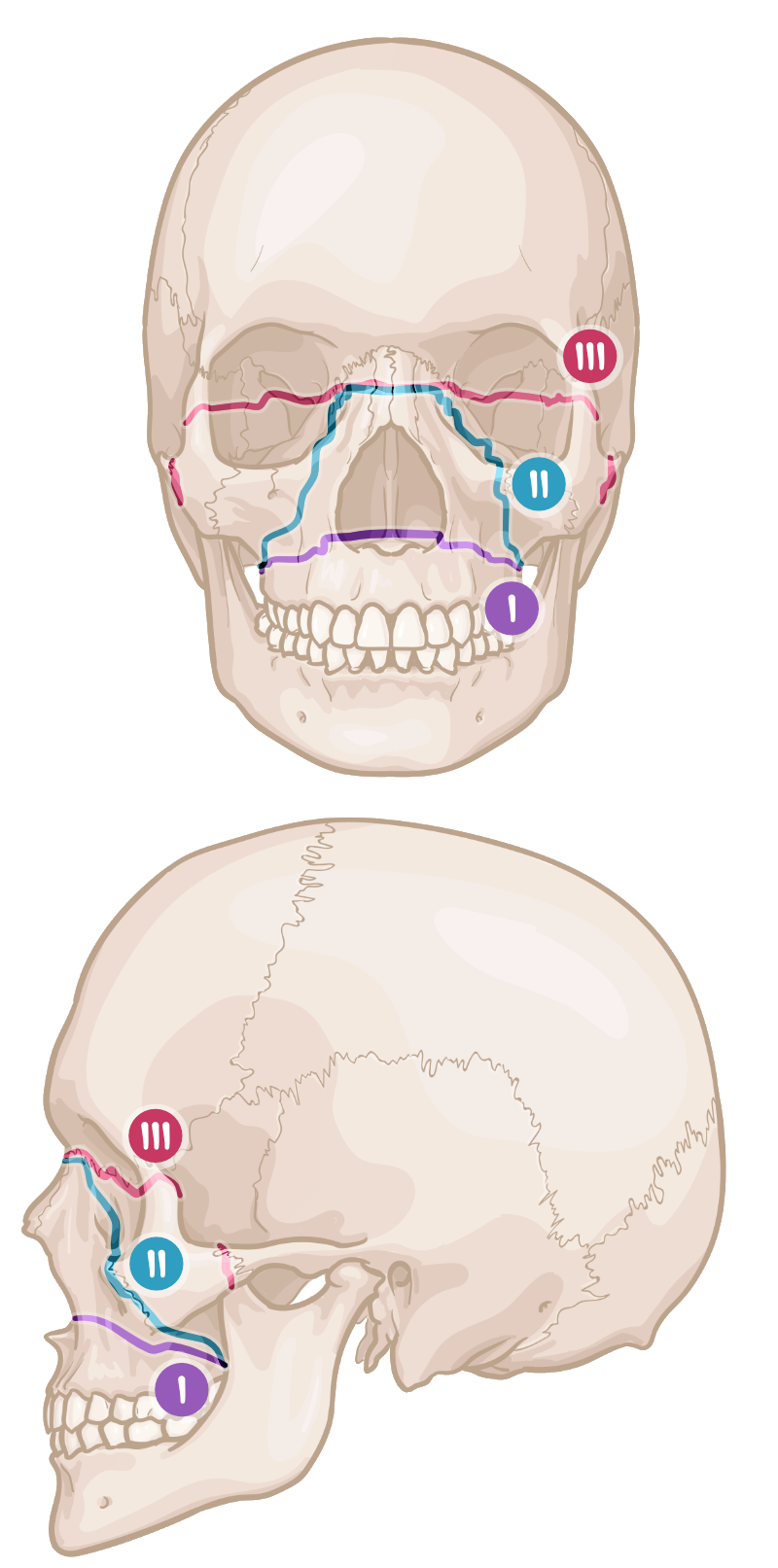
Occurs in a predictable fashion, giving rise to the Le Fort classification:- Le Fort I
Horizontal fracture of the maxilla at the plane of the nose.- Direct maxillary impact
- Le Fort II
Freely mobile pyramid of maxilla.- Most common fracture
- Inferior or lateral mandibular impact with a closed mouth
- Le fort III
Separation of midface from the base of the skull.- Also known as craniofacial disjunction
- May result in cribiform plate transection and CSF leak
- Le Fort I
Orbital fractures:
- Inferior orbital wall fracture most common
Direct pressure on globe is transmitted back to the orbit, with the weakest wall shattering. - May result in entrapment of globe or extra-ocular muscles
- Loss of visual acuity
- Abnormal eye movements
Aetiology
Facial injures are almost all related to blunt trauma; common causes include:
- MVA
- Assault
- Falls
- Sport
- Industrial accidents
Clinical Manifestations
Evaluation should include:
- Visible deformity
- Asymmetry
- Nasal septal deviation
- Fracture stability
- Palpation of midface for mobile segments
- Dental malocclusion
- Visual assessment
- Visual acuity
- Pupillary reflexes
- Eye movements
- Cranial nerve function
- Facial nerve
- Evidence of base of skull fracture
- Enopthalmos
Retraction of the eye due to blowout fracture. Upward gaze is usually impaired. - Bleeding
- Haemotympanum
- Battle’s sign
- Raccoon eyes
- Enopthalmos
- Orbital bruit
Suggests carotid-cavernous sinus fistulae.
Diagnostic Approach and DDx
Investigations
Bedside:
Laboratory:
Imaging:
Other:
Management
Airway management can be complex due to interplay of:
- Trauma
With effect of other injuries. - Oedema
- Haemorrhage
- Aspiration
- Impaired topicalisation
- Impaired
Resuscitation:
This details management of isolated midface injuries and implies reasonably normal laryngeal and tracheal anatomy.
Laryngotracheal trauma is rarer, and:
- Evidenced by stridor or hoarseness with overlying neck abnormalities
- Requires complex airway management strategies
- Covered under Laryngotracheal Trauma
- A
- Basic interventions
- Head-up position
Patient may assume unusual positions that limit obstruction, this should be encouraged. - High flow oxygen
- Regular suctioning
- Head-up position
- Advanced airway management
Planning should include senior airway clinicians. Considerations include:- Bag-mask ventilation often difficult
- Limited mask seal
- Pain
- Fibre-optic nasal intubation for mandibular condyle fracture with limited mouth opening, without base of skull fractures
- Non-condylar mandibular fractures are mobile when pain is controlled
- Awake oral fibre-optic intubation for:
- Cervical spine injury
- Mandibular condyle and base of skull fracture
- Awake tracheostomy may be considered
- Bag-mask ventilation often difficult
- Basic interventions
- C
- Bleeding
- Direct pressure
- Aggressive packing to wounds and nasal cavities
- Bleeding
Peculiar interventions that may assist airway patency include:
- Tongue protraction
Suture through anterior tongue allows tongue to be pulled forwards. - Midface protraction
Anterior traction of the mobile midface may relieve obstruction but ↑↑ venous bleeding.
Specific therapy:
- Pharmacological
- Prophylactic antibiotics
For CSF leak.
- Prophylactic antibiotics
- Procedural
- Angioembolisation
1st line for intractable bleeding. - Surgical haemorrhage control
- Debridement and washout
Within 24 hours. - Internal fixation
Often delayed 4-10 days until swelling has resolved.
- Angioembolisation
- Physical
Supportive care:
Disposition:
Preventative:
Marginal and Ineffective Therapies
- Steroids
No role in optic nerve injuyr.
Anaesthetic Considerations
Complications
Facial fractures have several associated injuries:
- A
- Dental injury
- C
- Carotid-cavernous sinus fistula
- D
- Cervical spine injury
- Intracranial injury
- Orbital injury
Vision loss or blindness in ~1%. - Base of skull fracture
- CSF leak
- Occurs in 10-30%.
- May present with either:
- Rhinorrhoea
- Otorrhoea
- Meningitis uncommon despite the prevalance of CSF leak
- CSF leak
Bones that may result in dural tears and CSF leak include:
- Frontal bone
- Frontal sinus
- Nasoethmoid complex
- Fronto-orbital complex
Prognosis
Key Studies
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.