Coagulation testing can be divided into tests of:
- Primary haemostasis
Formation of the initial platelet plug.
- Secondary haemostasis
Fibrin generation via the coagulation cascade.
- Global Coagulation
Holistic test of entire coagulation system function.
Primary Haemostasis
Defects of platelet plug formation can be due to either:
- Quantitative
Loss in absolute platelet number. Causes include:
- Consumption
- Bone marrow suppression
- Qualitative
Adequate platelet number but impaired function. Causes include:
- Drugs
- Aspirin
- Clopidogrel
- Ticagrelor
- Uraemia
- Hepatic cirrhosis
- Extracorporeal circuits
- Bone marrow dysfunction
- Multiple myeloma
- Myeloproliferative disorders
Platelet Count
Revealed by platelet count on an FBE:
- <50×109/L is significant in the presence of haemostatic failure
Platelet Function
Platelet function assays provide a qualitative assessment of platelet function, and are used for:
- Diagnosis of platelet disorders
- Monitor effect of antiplatelet therapy
Quantify response to GP IIb/IIIa inhibitors or clopidogrel.
Secondary Haemostasis
Assessment includes:
- Coagulation assays
- PT
- APTT
- TCT
- Mixing studies
- Fibrinogen
- Fibrinolytic assays
Prothrombin Time
Time taken for blood to clot after addition of tissue factor. The PT is:
- A test of the extrinsic pathway
- Prolonged by:
- Factor VII deficiency
- Liver disease
- Vitamin K deficiency
- Oral Xa inhibitors
- Used to calculate an INR
Normalises the PT calculation between laboratories so they can be accurately compared.
Activated Partial Thromboplastin Time
Also known as the Partial Thromboplastin Time (PTT), or historically as the kaolin-cephalin clotting time (KCCT).
Time taken for blood to clot after addition of some reagent. The APTT is:
I remember this as heparintrinsic, as heparin is measured using the APTT.
- A test of the intrinsic pathway
- Highly variable between laboratories
Normal ranges (including for anticoagulation with heparin) are variable.
- Prolonged by:
- Factor VIII, IX, or XI deficiency
- Contact phase deficiency
Does not result in clinically significant bleeding. Due to deficiency in:
- Oral thrombin inhibitors
Prolongation of both the PT and APTT may be due to deficiency of:
- Factor X or V
- Prothrombin (Factor II)
- Fibrinogen (Factor I)
Thrombin Clotting Time
Also known as Thrombin Time (TT).
Time taken for blood to clot after thrombin has been added. The TT is:
- A test of fibrinogen to fibrin conversion
- Prolonged by:
- ↓ Fibrinogen
- Dysfibrinogenaemia
- Heparin
- Presence of FDP
Reptilase Time
Time taken for blood to clot after addition of reptilase, which is:
Reptilase is also known as batroxobin, and is a haemolytic snake venom harvested from some aggressive species of the Bothrops genus of South American pit viper.
- Used as an adjunct to identify the cause of an ↑ TCT
- Normal with:
- Heparin
- Hirudin
- Direct thrombin inhibitor
- Prolonged by:
- Dysfibrinogenaemia
- Presence of FDP
Mixing Studies
Mixing studies involve combining equal parts normal donor plasma and patient plasma. Mixing studies:
- Can be performed for PT, APTT, and TCT
- Will correct if the coagulation abnormality is due to factor deficiency
- Will not correct if the abnormality is due to a factor inhibitor
- Direct thrombin inhibitors
- Acquired Factor VIII inhibitor
Acquired haemophilia A.
- Lupus anticoagulant
- Antiphospholipid syndrome
How much correction is required for result to be “corrected” is controversial:
- Large or multiple factor deficiencies may not correct with mixing
- Many patients have both deficiencies and inhibitors
- Some inhibitors are time-dependent
- Suggested indicators for adequate correction include the correct result:
- Entering the normal range
- Falling below some laboratory standardised value
Change of >70% is usually considered a correction.
The lupus anticoagulant is:
- A horrific misnomer, as it is not specific to either:
- A heterogenous antiphospholipid autoantibody
Predominantly both IgG and IgM.
- Present in:
- 2-4% of the general population
- 15-35% of patients with SLE
- A cause of arterial and venous thrombosis
- Indicated by an ↑ APTT that fails to correct on a standard mixing study, but does correct with addition of phospholipid
Fibrinogen
Fibrinogen is:
- ↑ In:
- ↓ In:
- Consumptive coagulopathy
- Hyperfibrinolysis
D-Dimer
The D-dimer is a measurement of FDP produced by fibrinolysis produced by the action of plasmin, and is ↑ with:
- Thromboembolism
- Post-operative
- Trauma
- AKI
- Sepsis
- DIC with hyperfibrinolysis
Global Coagulation Assays
Global assays include:
- Thromboelastography
- Thrombin Generation Tests
Thromboelastography
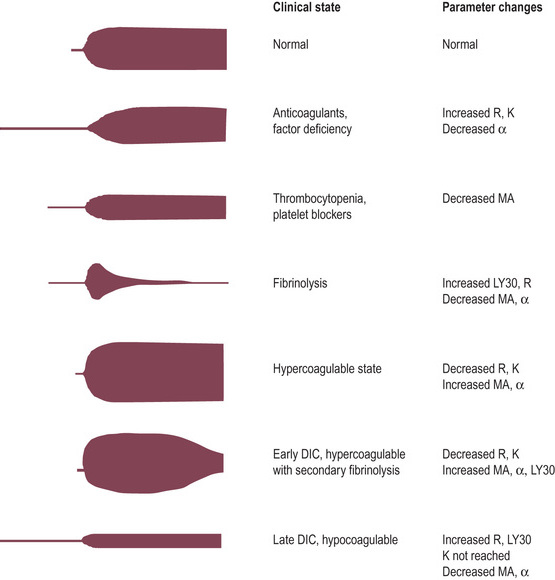
Thromboelastographic methods graph the changing strength and elasticity of a forming blood clot over time. These methods:
Due to the strong evidence supporting use of antifibrinolytics such as TXA in bleeding without strong evidence of harm, the utility of early detection of fibrinolysis is questionable since empiric treatment is safe.
- Include:
- TEG
Cup spins and pin remains stationary.
- ROTEM
Pin rotates and cup remains stationary.
- May have different additives to:
- Specifically test different aspects of clot formation
e.g. A heparinase channel, to estimate what clot strength would be in absence of heparin.
- Speed up test formation
- Advantages
- Real-time testing
Can be analysed as it progresses, rather than waiting for testing to be completed.
- Guide use of blood product including platelets, FFP, factor concentrates, and cryoprecipitate
- Give an early signal of the presence of fibrinolysis
Otherwise no strong evidence of benefit over traditional haemostatic testing.
- Disadvantages
- Additional training required to perform and interpret
- More expensive than traditional testing
Cost arguments are made that it saves excessive blood product use.
- Results do not translate directly to standard coag assays which are used in most guidelines for monitoring treatment
- Unclear what values should be targeted
- Measure various parameters including:
- R (Reaction) time (Clotting Time)
Time until initial fibrin formation.
- Efficacy of clotting cascade
- Prolonged R time indicates:
- Clotting factor deficiency
- Direct thrombin inhibition
- Heparin
- Prolonged R time treated with:
- Factor replacement
- Reversal of anticoagulant
- K (Kinetic) time/α-angle (Clot Formation Time)
Both index the time taken to achieve a certain level of clot strength.
- Prolonged K time indicates:
- Inadequate platelets
- Quantitative
Thrombocytopaenia.
- Qualitative
Platelet dysfunction.
- ↓ Fibrinogen
- Severe factor deficiency
Will also ↑ R time.
- ↓ α-angle or ↑ K time are treated with:
- Cryoprecipitate
- Platelets
- Maximum Amplitude (Maximum Clot Firmness)
Strength of platelet-fibrin interaction.
- ↓ MA indicates inadequate platelet function
- Treatment with:
- Platelets
- DDAVP
If qualitative defect.
- Lysis time
- Time taken until clot degrades by a certain percentage (e.g. LY30)
- Short lysis time treated with antifibrinolytics
The ROTEM definitions are listed in bold, the TEG equivalents are in parentheses.
DDAVP (desmopressin) is:
- A synthetic vasopressin analogue
- Dosed at 0.3μg/kg
- Response is variable between patients, but usually consistent for the one patient
- Tachyphylaxis occurs after 3-5 days
- Used for a variety of pro-coagulant effects:
- Release of stored vWF
Effective for mild quantitative and some qualitative von Willebrand disease.
- Release of factor VIII
Effective for mild haemophilia A.
- ↑ Platelet aggregation
- ↑ Surface GP receptors
- ↑ Platelet-dependent thrombin generation
Interpretation
Interpretation of Conventional Coagulation Assays
| Normal APTT |
- von Willebrand’s disease
- Platelet dysfunction
- Fibrinolysis
|
- ↓ Vitamin K dependent factors
- Warfarin therapy
- Vitamin K deficiency
- Liver disease
- Isolated Factor VII deficiency
|
| ↑ APTT |
Anticoagulant Factor:
- Normal TCT and Reptilase Time:
- Antiphospholipid antibodies
- ↑ TCT and normal Reptilase Time:
- Heparin
- Heparin-like anticoagulants
Malignancy.
- ↑ TCT and ↑ Reptilase Time:
- ↓ Fibrinogen
- Dysfibrinogenaemia
- Paraproteinaemia
- ↑ FDP
- Amyloidosis
Factor deficiency:
- von Willebrand’s disease
Functional factor 8 deficiency.
- Factor 8 deficiency
Haemophilia A.
- Factor 9 deficiency
Haemophilia B.
- Factor 11 deficiency
Haemophilia C.
- Factor 12 deficiency
|
Over-anticoagulation:
- Warfarin toxicity
- Direct thrombin inhibitor toxicity
- Post thrombolysis
- Snake bite
Other Coagulopathy:
- DIC
- Massive transfusion
- Severe liver failure
|
- ↑ APTT: Intrinsic pathway failure
- ↑ PT: Extrinsic pathway failure
Key Studies
Viscoelastic Testing:
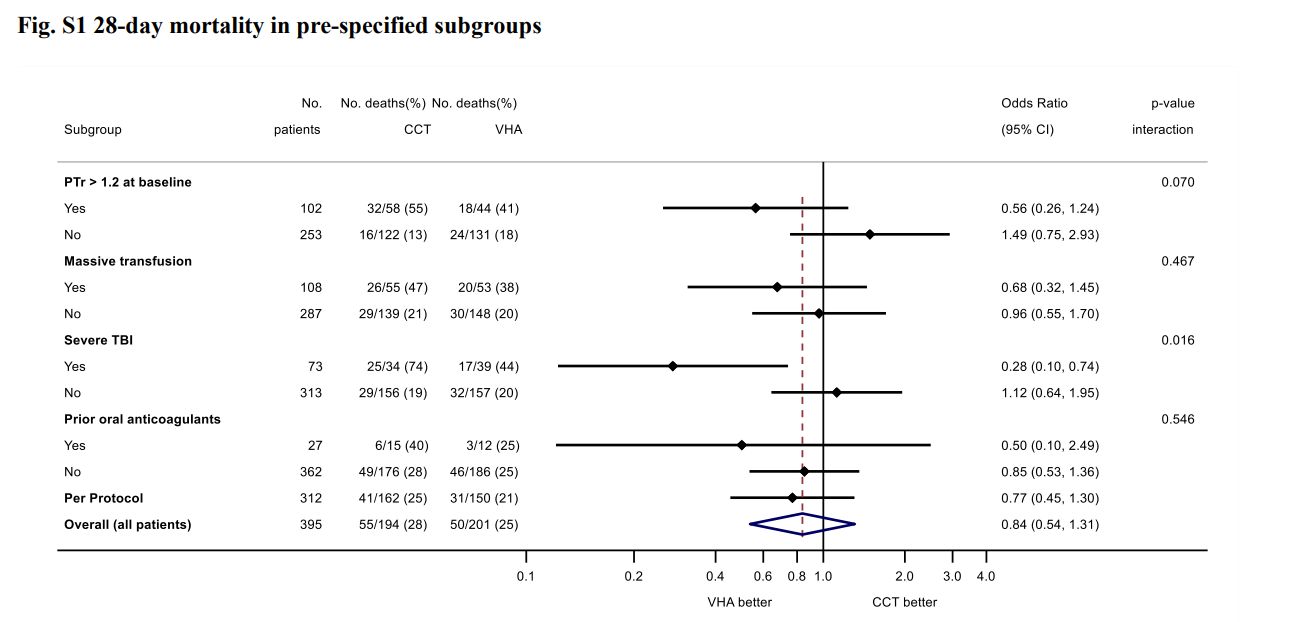
- ITACTIC (2020)
- 392 adult Europeans with trauma requiring MTP activation and active bleeding within 1 hour of ED admission and 3 hours of injury
- Block randomised multicentre (7), clinician unblinded, researcher blinded RCT
- 392 patients provides 80% for 15% ↓ in death or massive transfusion at 24 hours
- Viscoelastic assays (ROTEM or TEG) vs. conventional coagulation testing
- Protocolised treatment of coagulation abnormalities for both groups
- All patients received 1:1:1 transfusion, with algorithmic administration of TXA, fibrinogen, and additiojnal products
- Most patients severely injured
- No difference in primary outcome (67% vs 64%)
Ambitious difference for a monitoring trial.
- Secondary outcome supports 28 day mortality ↓ in TBI group