Malaria
Anopheles mosquito-borne protozoal infection endemic in tropical and subtropical regions, caused by four species of the Plasmodium genus:
- P. falciparum
- Most severe form
- Parasite-infected RBC may obstruct capillaries leading to localised tissue ischaemia and organ-dependent dysfunction
- P. vivax
- P. malariae
- P. ovale
Epidemiology and Risk Factors
Risk factors for malaria:
- Patient factors
- Age <3
- Non-immune
- Environmental factors
- Mosquito carrier
Specifically the female Anopheles, which are:- Night feeders
Dawn to dusk is the most dangerous time. - Rural breeders
Generally ↓↓ risk in urban areas, even in endemic regions.
- Night feeders
- Mosquito carrier
Severe malaria associated iwth:
- Children <5
- Non-immune travelers
- Immunosuppression
- Pregnancy
Pathophysiology
Life-cycle:
- Uninucleate sporozoites resident in mosquito salivary glands are injected into a human host during feeding
- Sporozoites rapidly invade liver parenchyma and mature into schizonts
- Bursting of schizonts releases 2,000 to 40,000 merozoites, each of which can infect a single RBC
- Maturation may take 1-2 years in P. vivax and P. ovale infections
- Merozoites mature in the RBC into either:
- Gametocyte
If ingested by a mosquito during feeding, will mature in the mosquito gut over 2-3 weeks into new sporozoites. - Erythrocytic schizont
Contain more merozoites; subsequent rupture releases merozoites and causes the cyclical fever.
- Gametocyte
The erythrocytic stage is the disease-causing stage; sporozoites and gametocytes are not associated with disease.
Sickled cells (see Sickle Cell Disease) haemolyse prematurely, interrupting the Plasmodium life-cycle.
Aetiology
Clinical Features
Presentations are divided into:
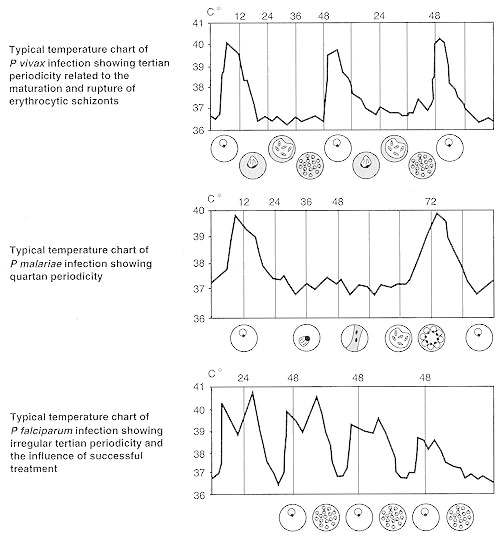
Cyclical symptoms occur when maturing malarial schizonts rupture their erythrocyte host, the timing of which varies on the strain:
- Tertian malaria
Maturation every 48 hours.- P. vivax
- P. ovale
- Quartan malaria
Maturation every 72 hours.- P. malariae
- P. Falciparum
Typically irregular fever spikes every 48 hours on the background of a continuous fever, but may also produce tertian malaria.
- Uncomplicated
Generic viral symptoms, progressing to classical cyclical fevers. - Severe malaria
Progression to organ dysfunction, most common with P. falciparum infection.
| Uncomplicated | Severe |
|---|---|
|
|
Cyclical fevers are the classical finding, and occur in three stages:
- 15-60 minutes cold shivering
- 2-6 hour fever (up to 41°C)
- 2-4 hour sweating
Normalisation of temperature.
Diagnostic Approach and DDx
Investigations
Bedside:
Laboratory:
- Blood
- FBE
- Normochromic normocytic anaemia
- Thrombocytopaenia
- LFTs
- UECs
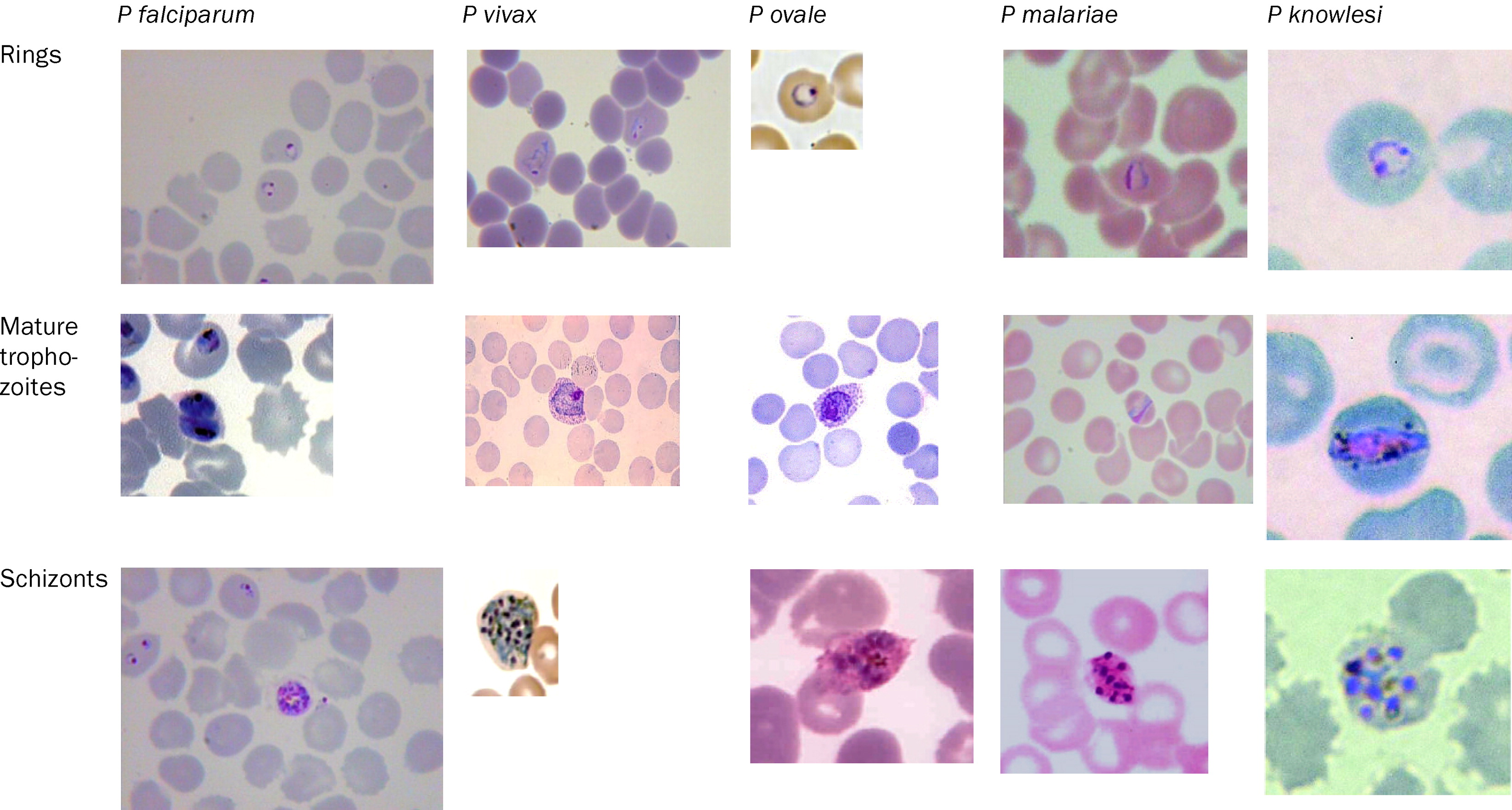
- Blood smears
Thick and thin films are gold standard of diagnosis:- Thin films identify parasites within red cells
- Thick films allow parasite counting
>10% of RBCs containing parasites indicates severe disease.
- Rapid diagnostic tests
Look for parasite-specific antigen. Qualitative evidence of disease. - Malaria PCR
More sensitive than antigen testing with similar limitations.
- FBE
Thick and thin films refer to the thickness of the blood on the slide.
Imaging:
Other:
Management
- Preventative antimalarials when visiting endemic areas
- Standard sepsis management
Covered under Management. - Antimalarials
Resuscitation:
- C
- Fluid boluses ↑ mortality in children
Specific therapy:
- Pharmacological
- Antimalarials
- Combination therapy recommended due to P. falciparum resistance
- Chloroquines kill mature parasites, immature parasites mature despite ongoing treatment
- Antimalarials
Preventative:
- Pharmacological
- Malarial prophylaxis
- Physical
- Mosquito nets
Marginal and Ineffective Therapies
- Steroids
Worsen outcome. - IVIG
Worsen outcome. - Exchange transfusion
Cytapheresis with replacement of native RBCs with donor RBCs, sometimes used if >10% parasitaemia. No indication of mortality benefit.
Anaesthetic Considerations
Complications
- B
- ARDS
- C
- Septic shock
- D
- Cerebral malaria
Mental status abnormality in a patient with malaria without another cause.- Due to obstruction of cerebral capillary blood flow, or efffect of malarial toxin
- Coma
- Convulsions
- ↑ ICP
- ↓ BSL
- Tone and postural abnormalties
Symmetrical pyramidal signs. - Retinopathy
- 15-50% mortality
- Cerebral malaria
- E
- Hypoglycaemia
- Electrolyte derangements
- Rhabdomyolysis
- F
- AKI
- ATN
Secondary to haemoglobinuria and rhabdomyolysis.
- H
- DIC
- Thrombocytopenia
Prognosis
Death associated with:
- Age <3
- Cerebral malaria
- Organ failures
- Anaemia
Key Studies
- FEAST (2011)
- 3170 African children aged 60 days to 12 years with febrile illness, ↓ conscious state, and ↓ perfusion; without malnourishment, gastroenteritis, or non-infectious shock
- Multicentre (6), un-blinded, allocation concealed, block-randomised trial
- 3600 patients would provide 80% power for 5% ↓ ARR of death, assuming control mortality of 11%
- Patients without severe hypotension (3141) randomised to one of:
- 20-40mL/kg 0.9% saline
- 20-40mL/kg 5% albumin
- No fluid
- Volumes of fluid were ↑ (from 20 to 40mL) after a protocol amendment partway through the trial
- Fluid groups received additional fluid if impaired perfusion
- All patients treated on general paediatric wards (no ICU available), and transfused if Hb <5g/dL
- 48 hour mortality was significantly ↑ in fluid groups
Saline 10.5%, albumin 10.6%, control 7.3%.- RR for saline vs. control: 1.44 (CI 1.09-1.9)
- Stopped early for harm
- Most deaths occurred at <24 hours
- Weaknesses:
- Clinical criteria for shock diagnosis are non-specific
- >50% had malaria, which behaves differently with IVT
- Significant anaemia may be made worse by haemodilution
A separate arm of FEAST protocolised management of severe hypotension, but there were only 29 patients and the discussion adds complexity disproportionate to insight so I have excluded it from this summary.
References
- Crutcher JM, Hoffman SL. Malaria. In: Baron S, editor. Medical Microbiology [Internet]. 4th ed. Galveston (TX): University of Texas Medical Branch at Galveston; 1996 [cited 2023 May 1].
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.
- Harvey RA, Cornelissen CN, Fisher BD. Lippincott Illustrated Reviews: Microbiology (Lippincott Illustrated Reviews Series). 3rd Ed. LWW.
- White NJ. Sharing malarias. The Lancet. 2004;363(9414):1006. doi:10.1016/S0140-6736(04)15879-0