Anaemia Overview
Pathological ↓ in the haemoglobin concentration of blood, resulting in a ↓ oxygen carrying capacity, and is:
- Defined as a (sea-level) haemoglobin of:
- ⩽130g/dL in men
- ⩽120g/dL in non-pregnant women
- ⩽110g/dL in pregnant women
- Classified by MCV into
- Microcytic
MCV⩽ 80fL. Major causes are:- Iron deficiency
- Congenital haemoglobinopathies
- Normocytic
MCV 80-96fL. Major causes are:- Anaemia of chronic disease
- Pregnancy
- Haemolysis
- Sickle-cell
- Macrocytic
MCV ⩾96 fL. Major causes are:- Folate/Vitamin B12 deficiency
- Alcohol
- Drug effect
- Microcytic
Epidemiology and Risk Factors
Anaemia in preoperative patients in Australia is:
- Common
- 6% of females
- 2% of males
- Risk ↑ with age
16% of patients over 75.
- Usually due to iron deficiency
Pathophysiology
Anaemia of inflammation occurs due to:
- ↑ Erythrocyte phagocytosis
Activated macrophages remove more red cells from circulation. - ↓ Erythropoiesis
Cytokines inhibit erythropoiesis, and may ↓ EPO expression. - ↓ Iron availability
Inflammation stimulates hepcidin release, which promotes iron trapping in marrow and erythrocytes.
Aetiology
| Microcytic | Normocytic | Macrocytic |
|---|---|---|
|
|
|
Clinical Features
Haemolysis:
- Infection
- Viral haemorrhagic fever
- Malaria
- Extracorporeal circuit
Assessment
History:
- Fevers
- Travel
Exam:
- Jaundice
- Haemoglobinuria
Investigations
Bedside:
Laboratory:
Red cell abnormalities and iron studies are covered in more detail under Erythrocytes and Iron Studies.
- Blood
- FBE
- Hb
- MCV
- MCHC
- RCC
- Blood film
- Haemolysis
- Sickle cells
- CRP
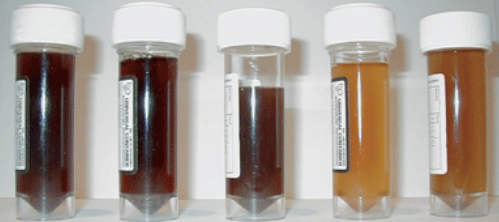
Performed if ferritin is raised in a microcytic anaemia, to exclude reactive causes. - Iron studies
- Ferritin
Assesses degree of iron deficiency.- Only reliable in absence of acute inflammation
Ferritin is an acute phase reactant - Normal range will depend on lab assay, but in general:
- Severe: ⩽30μg/mL
- Moderate: 30-50μg/mL
- Mild: 50-100μg/mL
- Only reliable in absence of acute inflammation
- Transferrin saturation
- <20% suggestive of iron deficiency
- Useful in moderate ferritin deficiency
- Ferritin
- Bilirubin
- Haemolysis screen
- Coagulation screen
- FBE
- Stool
- Faecal occult blood test
Coombs test is:
- Also known as antiglobulin testing
- A test for autoantibodies against circulating erythrocytes
- Diagnostic of autoimmune haemolytic anaemia
Also used in identifying transfusion-relevant antibody. - Performed either by:
- Direct antiglobulin testing
- Detects antibodies bound to erythrocytes.
- Patient blood washed in saline to remove plasma and unbound antibodies
- Reagent added to detect bound IgG
- Indirect antibody testing
- Patient plasma mixed with foreign erythocytes of known antigenicity
- Reagent added to detect patient antibody bound to foreign cells
- Direct antiglobulin testing
Haemolysis screen consists of:
- Reticulocyte count
↑ Due to ↑ marrow turnover. - Blood film
- Schistocytes
Mechanically fragmented erythrocyte, favours intravascular mechanical haemolysis.
- Schistocytes
- LDH
Present in many cells and so not specific for haemolysis (as opoposed to other cellular destruction). Substantial ↑ (4-5× ULN) favours intravascular over extravascular haemolysis. - Haptoglobin
Binds free haemoglobin, and is non-specific for intravascular vs. extravascular haemolysis. Acute phase reactant and so result may be equivocal in inflammatory states. - Free Hb
↑ Due to cellular destruction. - Bilirubin
↑ Due to haemoglobin metabolism. Classically ↑ conjugated bilirubin, although unconjugated may ↑ in concurrent hepatic impairment.
Imaging:
Other:
- Endoscopy
Diagnostic Approach and DDx
Management
Resuscitation:
Specific therapy:
- Pharmacological
- Iron supplementation
If iron deficient.- Oral
- Common
- Cheap
- Significantly limited by:
- Time
May take ⩾3 months of therapy to be effective, and 6-9 months for equivalent effect of one IV replacement. - Absorption
Highly variable. - Intake
- Non-compliance
Significant GI side effects.
- Time
- 80mg elemental iron given every second day
Daily administration down-regulates hepcidin, and reduces absorption.
- IV
Generally used if ferritin deficiency is severe, or moderate with low transferrin saturation.- Facilitate rapid repletion of stores
- Requires local pathway to facilitate
- Newer preparations have much lower incidence of anaphylaxis
Include iron polymaltose and iron carboxymaltose.
- Oral
- EPO
For renal anaemia without nutritional deficiency; generally requires nephrologist consultation. - Blood transfusion
- Iron supplementation
- Procedural
- Physical
Supportive care:
Disposition:
Preventative:
Marginal and Ineffective Therapies
Anaesthetic Considerations
Patients should be assessed 4-6 weeks pre-operatively.
The principles of patient blood management are covered under Patient Blood Management.
Complications
Prognosis
Anaemia is an independent risk factor for:
- Mortality
- Morbidity
- Hospitalisation
- ↓ Quality of Life
Key Studies
References
- Tefferi A. Anemia in Adults: A Contemporary Approach to Diagnosis. Mayo Clinic Proceedings. 2003;78(10):1274-1280. doi:10.4065/78.10.1274