Legionellosis
The pneumonic form of legionellosis is also known as Legionnaires’ disease, and the non-pneumonic form as Pontiac fever. This section focuses on the pneumonic form.
Legionellosis is an umbrella term encompassing infection with the Legionella bacterium which is transmitted by inhalation of aerosols from contaminated water or soil, and is divided into:
- Pneumonic form
- 2-10 day incubation
- Constitutional symptoms
- Mild to severe pneumonia
- Haemoptysis is common
- 5-10% mortality
- Weeks-months duration
- Non-pneumonic form
- 4-48 hour incubation
- Acute, self-limiting flu-like illness
- 2-5 day duration
Epidemiology and Risk Factors
Epidemiology:
- ~2/100,000
- 1-10% of CAP
Risk factors:
- Age
- Male
- Smoking
- Heavy alcohol use
- Pulmonary disease
Pathophysiology
Legionella is:
- Gram negative
- Aerobic
- Intracellular
- May also infect protozoa
- Aspirated bacteria attach to alveolar macrophages and epithelium
- Fastidious
Aetiology
Transmission occurs via inhalation of contaminated aerosols from contaminated water, and not by human-human transmission. There are >60 strains; key pathogenic strains include:
- L. pneumophila
- National and artificial systems
- Grow at 20-50°C
- Contamination occurs when changes in water behaviour disrupt biofilms, releasing a bacterial bolus into the water
- Most prevalent strain
Serotype 1 causes >80% of all cases worldwide.
- National and artificial systems
- L. longbeachae
- Potting mixes
- Soil
- Second most prevalent strain
Particularly in Australia and New Zealand.
- L. micdadei
- L. bozemanii
- L. feeleii
- L. anisa
- L. dumoffii
Possible sources include:
- Air conditioning cooling towers
- Hot and cold water systems
- Humidifiers
- Whirlpool spas
- Water birth
Assessment
Common clinical features include:
- Flu-like symptoms
- Fever/chills
- Myalgias
- Tiredness
- Headache
- Anorexia
- Cough
- Sore throat
- Rhinorrhoea
- Nausea
- Vomiting
Fever and fatigue typically proceed the onset of cough.
Extra-pulmonary infections are rare, but may include:
- Cellulitis
- Abscesses
- Endocarditis
- Meningitis
History
Examination
- Crepitations
Investigations
Bedside:
Laboratory:
- Blood
- FBE
- LFT
- ↑ ALT/AST
- UEC
- ↓ Na+
- CRP >100
- Sputum
- Deep respiratory sample PCR
Preferred diagnostic test as it detects all species and has high diagnostic accuracy. - Culture
- Requires rapid processing
Poor survival in secretions.
- Requires rapid processing
- Deep respiratory sample PCR
- Urine
- Antigen
Only detects L. pneumophila serotype 1.
- Antigen
Imaging:
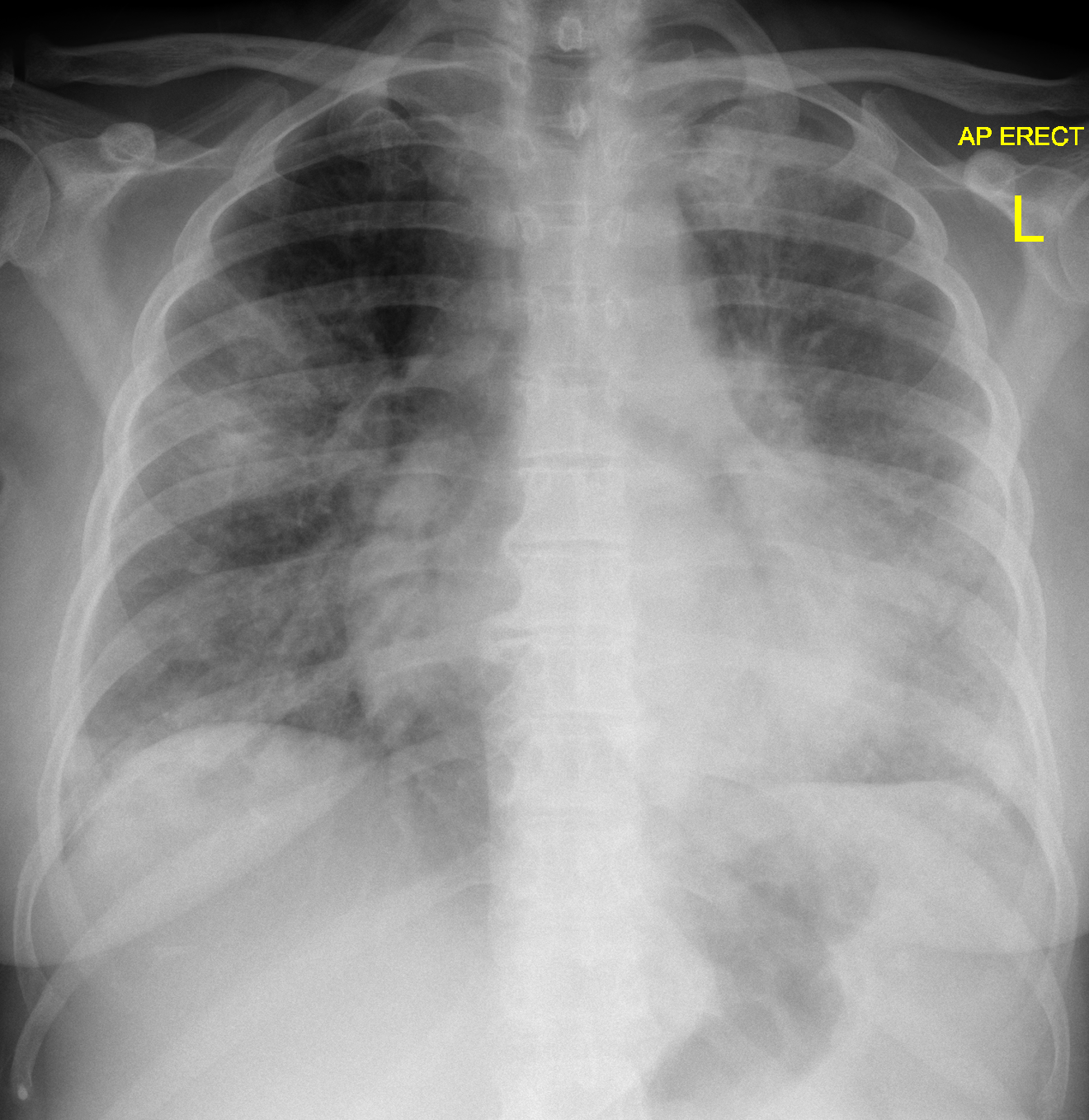
- CXR
- Patchy unilobular infiltrates
Other:
Diagnostic Approach and DDx
Legionnaire’s disease should be considered in any patient with:
- Moderate-severe pneumonia
- Possible exposure to Legionella
- Immunocompromise
Features differentiating Legionnaire’s disease from other causes of CAP include:
- GIT symptoms
- ↑ ALT/AST
- ↓ Na+
- CRP >100
- Failure to respond to beta-lactam monotherapy
Management
- Early antimicrobial therapy
- Respiratory support
Resuscitation:
Specific therapy:
“Atypical cover” in standard empiric CAP regimens are designed to cover (among others) Legionella, and is covered in detail under Pneumonia. Note that unlike fluoroquinolones, macrolides or tetracyclines alone do not provide adequate empiric CAP cover.
- Pharmacological
- Antimicrobial
5-day course of either:- Macrolide
- Azithromycin 500mg PO load, then 250mg PO daily
- Clarithromycin 500mg PO BD, then 1g PO daily
- Tetracycline
- Doxycycline 100mg PO BD
L. longbeachae is commonly resistant.
- Doxycycline 100mg PO BD
- Fluoroquinolones
- Levofloxacin
- Moxifloxacin
- Macrolide
- Antimicrobial
- Procedural
- Physical
Macrolides are preferred because they are bactericidal, have excellent pulmonary tissue penetration, and are active against all pathogenic strains.
Supportive care:
Disposition:
Preventative:
- Water safety plans
- Regular maintenance
- Drift eliminators
↓ Aerosol dissemination. - Biocide use
e.g. Chlorine. - Temperature control
- Hot water >50°C
- Cold <25°C
Ideally <20°C.
- Flush water sources regularly
- Work with soil in a well ventilated area
Marginal and Ineffective Therapies
Anaesthetic Considerations
Complications
- Death
- 5-10%
- Up to 40% in immunocompromised
Prognosis
Key Studies
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.
- World Health Organisation. 2022. Legionellosis [Fact Sheet].
- Thibodeau KP, Viera AJ. Atypical Pathogens and Challenges in Community-Acquired Pneumonia. American Family Physician. 2004 Apr 1;69(7):1699–707.
- Case courtesy of Henry Knipe, Radiopaedia.org. From the case rID: 31816.