Pneumonia
Infection of pulmonary parenchyma that is:
Systemic symptoms are much less common in the elderly and may be absent.
Non-respiratory symptoms may also be present.
- Defined by presence of both:
- Symptoms of acute infection
- Evidence of pulmonary infiltrate
- Radiographic
- Clinical
Crepitations, etc.
- Divided by epidemiology into:
- Community Acquired Pneumonia
Pneumonia in a patient who was not hospitalised prior to the onset of symptoms. - Nosocomial Pneumonias:
- Hospital Acquired Pneumonia
Pneumonia within 48 hours of hospital admission. - Ventilator Acquired Pneumonia
Pneumonia within 48 hours of intubation.
- Hospital Acquired Pneumonia
- Community Acquired Pneumonia
VAP is ventilator-associated, i.e. there is no requirement to demonstrate causality.
“Atypical” pneumonia describes infection that is:
- Responsible for up to 40% of CAP
- Caused by organisms that are less detectable on Gram stain
Including:- M. pneumoniae
- C. pneumoniae
- L. pneumophilia
- Coxiella burnetti
- Dominated by constitutional, rather than respiratory, symptoms
- Generally milder
- Not covered by ß-lactams
Requires treatment with macrolides or tetracyclines.
Epidemiology and Risk Factors
CAP has an annual incidence of up to 4% of the population:
- 50% require hospital admission
- Mortality 10% among the hospitalised group
- 10% require ICU admission
HAP:
- Occurs in 0.5-5% of inpatients
VAP:
- 8-30% of mechanically ventilated patients
- ~3%/day over first 5 days, with a decline thereafter
- 25-50% mortality
- Earlier infections are typically less-resistant and therefore more treatable than late-developing VAP
Risk factors:
- Immunocompromised
- Critically unwell
- In ICU
- Diabetes
- Advanced age
- Critically unwell
- Microaspiration
- Intubated
- ↓ Conscious state
- NGT in situ
- Pathology
- Chronic lung disease
- Receiving antibiotics
- Procedural
- Post-operative
- Bronchoscopy
- Thoracic surgery
- Abdominal surgery
- Environmental
- Local biogram
- Regular ventilator tubing changes
Pathophysiology
Proposed mechanisms include:
- Microaspiration of upper respiratory tract colonisers
- Local spread
- Haematogenous spread
Aetiology of Community Acquired Pneumonia
There are vast numbers of potentially causative organisms, however the most common in patients requiring ICU admission are:
- Viral
25%, most commonly:- RSV
- Influenza
- S. Pneumoniae
- H. Influenzae
- Legionella spp.
- Enterobacteriaceae spp.
- S. aureus
- Pseudomonas spp.
Staphylococcal infections are covered in detail under Staphylococci. Legionellosis is covered under Legionellosis.
Factors favouring infection with certain organisms include:
- Exposures
- Animal
- Animal exposures
- Birds and excreta
- Parturient pets or farm animals
- Insect bites
- Mice and excreta
- Bats and excreta
- Geographical factors
- TB prevalence
- Locally endemic organisms
- Animal
- Patient factors
- IVDU
- Alcoholism
- Respiratory disease
- COPD
- CF
- Bronchiectasis
- Other disease
- Diabetes
- Sickle cell
- Poor dental hygiene
- Immunosuppression
- Disease factors
- Sputum smell
- Lung abscesses
- Empyema
Aetiology of Nosocomial Pneumonia
Broadly, three classes of infection can occur:
- Most common
Aerobic gram negative bacilli:- Klebsiella spp.
- E. coli
- Pseudomonas spp.
- Early-onset
VAP within 5 days is more likely to include a wider array of community pathogens:- MRSA
- S. pneumoniae
- H. influenzae
- Late-onset
After 5 days, exogenous MRO may be seen:- MRSA
- P. aeruginosa
- Acinetobacter baumannii
- S. maltophilia
Risk factors for MRO include:
- Disease
- Immunosuppression
- Bronchiectasis
- Septic shock
- ARDS
- Treatment
- Prior IV ABx in previous 90 days
- Hospitalisation >5 days
- RRT
- Environmental
- High local MDR burden
Assessment
May be either:
- Systemic
- Fever
- Sweats
- Rigors
- Respiratory
- Productive cough
- Pleural rub
- Inspiratory crepitations
Clinical signs of respiratory infection without CXR infiltrates are suggestive of tracheobronchitis.
History
- Prognostic factors
- Cardiopulmonary
- Smoking
- COPD
- CCF
- Pulmonary hypertension
- Exercise tolerance
- Immune function
- Immunocompromise
- Vaccinations
- Malignancy
- Chemotherapy
- Other organ failures
- Cardiopulmonary
- Aetiology
- Country of origin
- Travel history
- TB exposure
- Recent hospital admission
- Recent antibiotic use
- Activities
- Gardening
- Bushwalking
- Animal exposure
- Birds
- Pets
Examination
Investigations
Laboratory:
- Blood:
- FBE
WCC may ↑ or ↓. - UEC
- LFT
- Blood cultures (×2-3)
- Procalcitonin
May have a role in timing deescalation of antibiotics. - CRP
- Prognostic
- ↑ CRP identifies a subgroup that demonstrate ↑ benefit from steroids
- HIV status
- FBE
- Sputum:
- Tests include:
- Gram stain
- Culture
Neither sensitive nor specific; more accurate results seen with:- Induced sputum
- Deep tracheal suctioning
- BAL
- Mycoplasma pneumoniae PCR
- Chlamydophila PCR
- Influenza PCR
- Legionella PCR
- COVID PCR
- Collection is ideally:
- From a deep cough
- To minimise contamination from upper respiratory tract commensals More complex in the intubated patient; options (in order of preference) include:
- Tracheal aspirate
Identify potentially causative organisms but is not quantitative. - Bronchial washings
- Bronchoalveolar lavage
- Prior to antibiotics
- Tracheal aspirate
- To minimise contamination from upper respiratory tract commensals More complex in the intubated patient; options (in order of preference) include:
- From a deep cough
- Rapid transport to laboratory ↑ chance of detecting fastidious organisms
- Causative organism is likely if:
- Dominant on gram stain
- Heavy growth on culture
- Tests include:
- Urine:
- Legionella antigen
- Highly specific but not sensitive for infection
Only detects Legionella pneumophilia, and not other pathogenic strains.
- Highly specific but not sensitive for infection
- Pneumococcal antigen
- Highly specific and moderately sensitive
- Unaffected by antibiotic therapy
- Level correlates with severity
- May have a role in narrowing spectrum of treatment to penicillin alone
- Legionella antigen
Anaerobic culture cannot be performed on sputum due to contamination from other upper respiratory organisms.
Interpretation of sputum cultures is fraught due to the amount of contamination with oropharyngeal flora. Tracheal aspirate or BAL is preferable.
The primary role of sputum culture in HAP/VAP is to identify resistant organisms and allow de-escalation to a narrower spectrum when the resistance profile is determined.
Imaging:
- CXR
- Infiltrates required for diagnosis is many guidelines, although may be absent in up to 25%
- Appearance usually worsens in initial period, even with institution of appropriate antibiotics
Features of concern are:- Cavitation
- Pleural effusion
- Radiographic improvement lags behind clinical response
- CT
More sensitive than CXR. - Lung ultrasound
Diagnostic Approach and DDx
Several tools exist to determine severity:
- CURB-65
Good for identifying low-mortality patients, more useful in ED and GP practices.- Consists of:
- Confusion
- Urea >7mmol/L
- Respiratory rate ⩾30
- SBP <90mmHg or DBP <60mmHg
- Age ⩾65
- Interpretation:
Mortality increases with each additional point.- 0-1: Low risk: Consider home treatment
- 2: Intermediate risk: Closely supervised outpatient treatment +/- hospitalisation
- >3: High risk: Hospitalise +/- ICU.
- Consists of:
- SMART-COP
Better at determining disposition, including need for ICU care.- ⩾4 has 1/3 chance of requiring vasoactive or respiratory support
- Consists of:
- SBP <90
- Multilobar infiltrate
- Albumin <35g/L
- RR:
- >30 if age >50
- >25 if age >25
- Tachycardia >125
- Confusion
- Oxygen saturation <93%
- pH <7.35
Other scores include the Pneumonia Severity Index, which is similar to CURB65.
Management
- Respiratory support
- Early antimicrobials
- Standard sepsis management
Covered under Management.
Resuscitation:
- A
- Intubation
For respiratory failure.
- Intubation
- B
- High-flow oxygen
- NIV
- Beneficial if there is pneumonia superimposed on another cause of respiratory failure that is manageable with NIV (e.g. APO)
- Unhelpful in isolated pneumonia due to ↓ cough efficacy
- Mechanical ventilation
If requiring intubation.
- C
- Haemodynamic support if concurrent sepsis
Specific therapy:
- Pharmacological
- Antimicrobial therapy
- CAP:
- Non-tropical
- Mild:
5-7 days of:- Amoxicillin 1g PO TDS
- Clarithromycin 250mg PO BD
- Moderate:
7-10 days of dual therapy, either:- Benzylpenicillin 1.2g IV QID and doxycycline 100mg PO BD
- Ceftriaxone 1g IV daily and doxycycline 100mg PO BD
- Severe:
7-10 days of dual therapy, either:- Ceftriaxone 1g IV daily and azithromycin 500mg IV daily
- Benzylpenicillin 1.2g IV Q4H and gentamicin
- Mild:
- Tropical
To cover Burkholderia pseudomallei and Acinetobacter baumannii:- Meropenem 1g IV TDS and azithromycin 500mg IV daily
- Non-tropical
- HAP/VAP:
- 7 day course recommended to reduce subsequent MDR pneumonias.
- 2-3 days until clinical response seen is usual
- If failing to respond, consider:
- Wrong bug
Repeat cultures. - Wrong drug
Ensure sensitivity of organism to the antibiotic being used. - Wrong dose
Appropriate for patient weight. - Sequestration
Abscess cavity or similar - Patient factors
- Immunosuppression
- Frailty
- Wrong bug
- No MDR risk factors
Consider:- Tazocin 4.5g Q6-8H
- Cefepime 2g Q8H
- Meropenem 1g Q8H
- MDR risk factors
Consider one of each of:- Antipseudomonal broad spectrum agent
As above. - Additional gram negative cover
↓ Risk that pathogen is resistant to the primary agent.- Aminoglycoside 15-20mg Q24H
- Ciprofloxacin 400mg Q8H
- Levofloxacin 750mg Q24H
- MRSA cover:
- Linezolid 600mg Q12H
Preferable due to better pulmonary penetration. - Vancomycin
- Linezolid 600mg Q12H
- Antipseudomonal broad spectrum agent
- Nebulised antibiotics
Appropriate in limited circumstances, namely all of:- VAP
- Multi-resistant Gram negative
Sensitive only to:- Aminoglycosides
- Colistin
- CAP:
- Hydrocortisone
- Probable mortality benefit
- Suggest 200mg/day for 4-7 days, followed by 3-7 days of weaning
- Unless contraindicated
- Chronic infection
- Immunocompromised
- Poorly controlled diabetes
- Pregnancy
- Antimicrobial therapy
- Procedural
- Bronchoscopy
- Diagnostic sampling
- For segmental or lobar collapse
- Bronchoscopy
- Physical
Antimicrobial therapy is often unit or region-specific based on local flora and resistance patterns.
Failure of treatment response is usually due to a resistance Gram positive, e.g. S. pneumoniae, and so broadening Gram negative cover from ceftriaxone to tazocin is not helpful.
Up to 40% of patients have a polymicrobial infection, so narrowing the spectrum of cover following identification of an organism may result in inadequate treatment.
Nebulisation of antibiotics is:
- Pharmacologically justified by:
- Achieving ↑ drug concentration at site of infection
- Most antibiotics have poor lung penetration
- ↓ Systemic dose and therefore toxicity
- Limited by:
- Uncertain dose delivered
- Binding of drug to circuit filter
- Complications of excipients
- Lack of strong evidence
- Recommended only for:
- Colistin
A reasonable approach to hydrocortisone therapy, including weaning, is included in the summary of the CAPE COD trial; see Key Studies.
Supportive care:
- B
- Supplemental oxygen
- Chest physiotherapy
- Sitting position
- Bubble PEEP
- Encouraging coughing
Disposition:
- ICU or HDU for severe disease
Prevention:
- A
- Nurse 30° head up to ↓ risk of microaspiration
- Oral care Q4H with chlorhexidine mouthwash BD
- Use cuff-pressures
- Use subglottic suctioning
- Use closed suction circuits
- Avoid non-essential suctioning
- Intubate orally (rather than nasally)
- Minimise changes of ventilation equipment
- Suction catheters
- Humidifiers
- Circuit
Weekly intervals.
- B
- Minimise duration of mechanical ventilation
- E
- Early mobilisation
- G
- SDD
- Post-pyloric feeding
- Avoid NG tubes
OG tubes are preferable.
Marginal and Ineffective Therapies
Complications
- Nosocomial pneumonias ↑ hospital LoS by ~13 days
- B
- Parapneumonic effusion
- Uncomplicated effusions resolve with resolution of the underlying infection
- Complex effusions:
- Develop 1-2 weeks after the initial fluid collection
- May occur with persistent fevers and have organisms on Gram stain
Essentially empyema-lite.
- Empyema Collection of pus in the pleural space, usually evolving from a parapneumonic effusion. Antibiotics are adjunctive - these require drainage.
- Cavitating pneumonia
Parenchymal destruction leading formation of gas filled space or pneumothorax, and is associated with infection with:- S. aureus
- S. pneumoniae
- H. influenzae
- K. pneumoniae
- P. aeruginosa
- Fungal pneumonias
- Atypical mycobacterium
- Persistent pneumonia Pneumonia unresponsive to 5 days of appropriate antibiotic therapy, which should stimulate search for an alternate diagnosis or signs of a complicated infection.
- Parapneumonic effusion
Empyema and non-responsive pneumonias are covered in more detail under Empyema and ?sec-pers_pneumonia.
Persistent Pneumonias
Failure to improve after an arbitrary 5 days of treatment should prompt consideration of:
Risk factors for persistent pneumonia:
- ↑ Age
- Comorbidities
- Chronic respiratory disease
- Lifestyle
- Hight alcohol intake
- Smoking
- Pneumonia
- Multilobar
- Bacteraemia
- Infected collections
- Organisms
- Legionella
- Polymicrobial
- A broader differential:
- Wrong disease
- Vasculitis
- Malignancy
- Diffuse alveolar haemorrhage
- Alveolar proteinosis
- Heart failure
- Sarcoidosis
- Eosinophilic pneumonia
- Interstitial pneumonia
- Wrong drug/bug
- Resistant organism
- Atypical organism
- Viral pneumonia
- Wrong dose
- Underdosing
- Inappropriate dose interval
- Poor penetration
- Underdosing
- Failure of source control
- Wrong disease
- Further investigations:
- Sputum
- Eosinophils
- Acid-fast bacilli
- Viral PCR
- BAL
- TTE
- Endocarditis
- LV failure
- High-resolution CT Chest
- Cavitations
- Loculated collections
- Bronchial masses
- Pneumonic characteristics
- Sputum
- Lung biopsy
- Highly invasive
- Significant procedural risk
- May be appropriate when:
- No other clear diagnosis
- Failure of empirical therapy
- Potential treatments are:
- Morbid
- Mutually incompatible
- Useful for determining:
- Presence of idiopathic interstitial pneumonia, e.g.:
- Cryptogenic organising pneumonia
- Acute interstitial pneumonia
- Absence of:
- Sarcoidosis
- Hypersensitivity pneumonitis
- Pulmonary histiocytosis
- Presence of idiopathic interstitial pneumonia, e.g.:
Prognosis
Time until improvement varies:
- Average ~3 days
- 7 days in the:
- Elderly
- Bacteraemic
- 2.5 days in young patients with pneumococcal pneumonia
Poor prognostic signs follow logically:
The PaO2:FiO2 (P:F) and SpO2:FiO2 and (S:F) ratios quantify the degree of hypoxia relative to the degree of oxygen supplementation.
They are calculated as:
- \(P/F = {PaO_2 \over FiO_2}\)
- \(S/F = {SpO_2 \over FiO_2} \times 1000\)
Where:
- \(PaO_2\) is in mmHg
- \(FiO_2\) is a decimal (0-1)
- Severity of respiratory failure
- Invasive mechanical ventilation
- RR >30
- P/F <250
- Severity of sepsis
- Septic shock
- Leukopenia
- Thrombocytopenia
- Hypothermia
Key Studies
Steroids:
- LRTI alters alveolar membrane permeability
- Local inflammatory response
- Systemic inflammatory response
- Immunomodulation potentially therapeutic
- Ceftriaxone ↑ inflammation in S. pneumoniae (pneumonococcus) infection
- CAP is a heterogenous disease with a variety of different causative organisms and degrees of severity
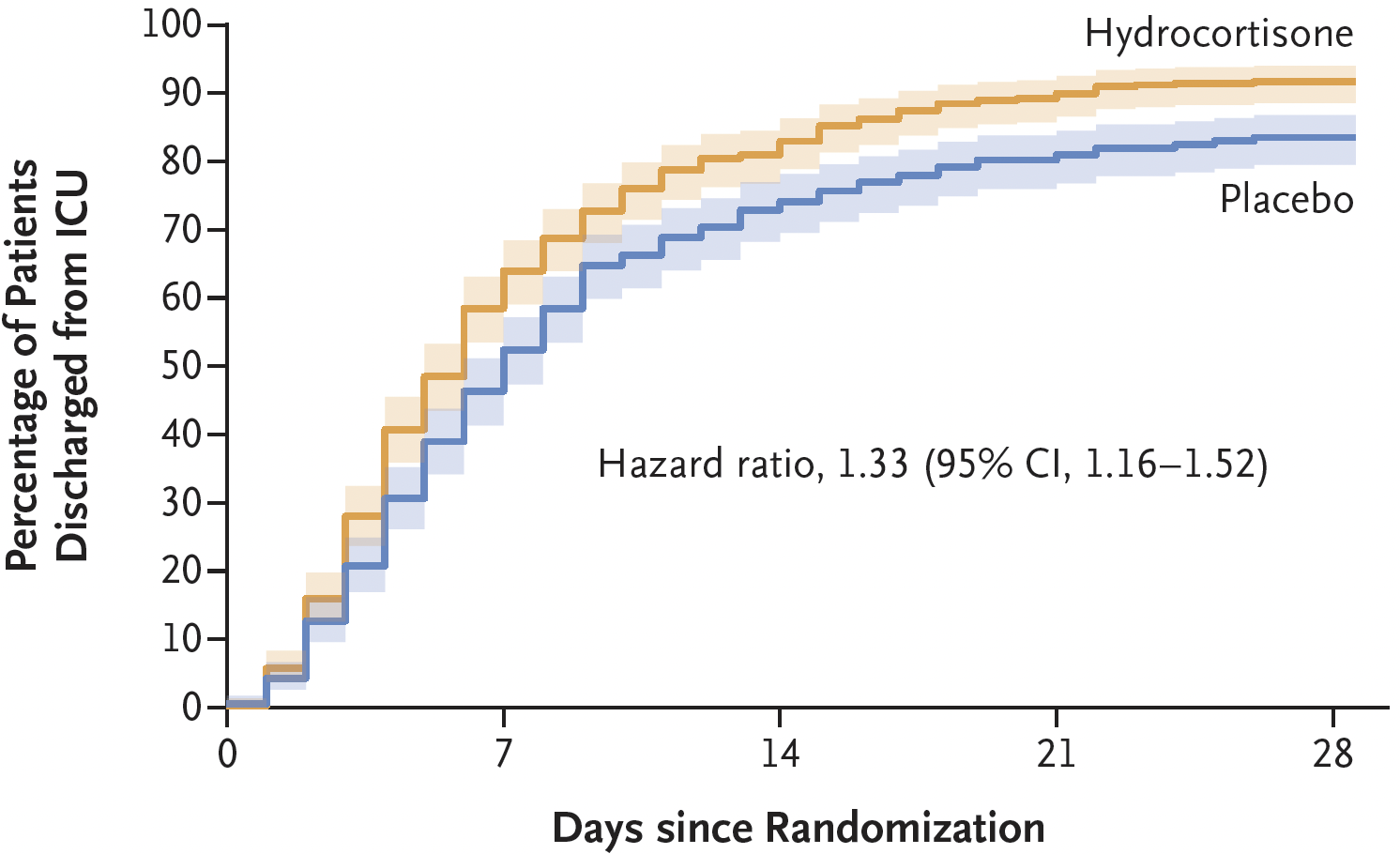
- CAPE COD (2023)
- 800 French ICU patients with severe CAP
- Without septic shock
- Without features suggesting other causes of pneumonia mimics
- Hydrocortisone infusion vs. placebo
- 200mg/day for 4 days
- Decision made at day 4 for either a short or long course
Based on severity of illness, P/F ratio, respiratory wean, and expected ICU LoS.- Short course
100mg/day for 2 days, then 50mg/day for 2 days (total 8 days). - Long course 200mg/day for further 3 days, then 100mg/day for 4 days, then 50mg/day for 3 days (total 14 days).
- Short course
- Significant:
- ↓ Mortality in treatment group (6.2% vs. 11.9%)
- ↑ Insulin use in treatment group
- Stopped early due to COVID and significance on interim analysis
- 800 French ICU patients with severe CAP
References
- Bersten, A. D., & Handy, J. M. (2018). Oh’s Intensive Care Manual. Elsevier Gezondheidszorg.
- Dequin PF, Meziani F, Quenot JP, et al. Hydrocortisone in Severe Community-Acquired Pneumonia. N Engl J Med. Published online March 21, 2023:NEJMoa2215145.
- Parkar AP, Kandiah P. Differential Diagnosis of Cavitary Lung Lesions. J Belg Soc Radiol. 100(1):100.